By: Mohamed Nezar Abohalawa. Cairo, Egypt. DLHA Volunteer and Freelance Health writer; with medical review and editorial support by the DLHA Team.
·Appendicitis (or inflamed appendix) is the commonest cause of abdominal emergencies globally.
The lifetime risk of appendicitis in Africa is low (1.8%) compared to other areas of the world.(8)
The annual incidence of appendicitis in Nigeria for example is reported to be 22.1– 49.8 new cases per 100,000 population. Males are more affected than females. (8)
Migratory pain that eventually localises to the right lower abdomen is the dominant symptom of appendicitis. Others include fever, nausea, vomiting and general unwellness.
The best and prompt treatment of appendicitis is through surgical removal.
Delayed or poorly treated appendicitis carries grave consequences.
Appendicitis simply means “inflamed appendix”. Before we learn about this condition, it would be helpful to know more about the appendix itself.
The word appendix dates back to the mid-16th century, and it is derived from the English word “Appendage” which originates from the Latin word “Appendare”, which means to add a note at the end of a document, or something attached to another bigger thing.
Interestingly, the appendix is an extension attached to one end of the large intestine!
So, what is the function of the human appendix? Is it true that it is useless in the body? Is it true that it is commonly inflamed?
Let’s dive in to find answers to these questions and more.
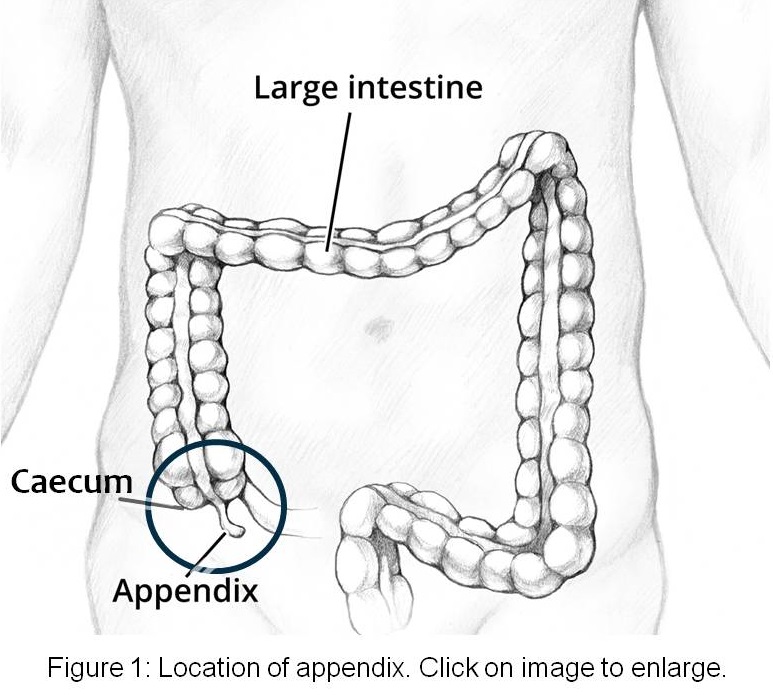 The appendix is a thin tube of about 4 inches. It’s attached to a pouch of the large intestine called the cecum. The cecum – which lies in the right lower part of your abdomen - marks the beginning of the large intestine. See figure 1 (1)
The appendix is a thin tube of about 4 inches. It’s attached to a pouch of the large intestine called the cecum. The cecum – which lies in the right lower part of your abdomen - marks the beginning of the large intestine. See figure 1 (1)
After years of thinking that the appendix was just a rudimentary structure with no meaningful function, scientists discovered that the appendix contains many immune cells, suggesting a role in fighting infection.
In addition, some components of the appendix (i.e., lymphatic tissue) help beneficial bacteria to thrive if they are wiped out by a microbe.
However, the exact function is still unknown.
Yes, the appendix is the commonest part of the bowel that gets inflamed. In fact, this condition is a global issue, being the most common cause of surgical operation on the abdomen. (2)
In Africa, 1 out of 55 Africans will develop appendicitis. Males appear more affected, and the lifetime risk is 1.8%. Evidence suggests that the burden of this condition is rising in the African general population. (3, 4)
The dangerous impact of appendicitis is not due to the disease itself, it’s surprisingly an issue of a patient seeking medical care after it’s too late.
Studies from one African community show that over 80% of patients presented in hospital later than 24 hours of onset of symptoms. (8)
You may diagnose a group of 1000 patients with early appendicitis and they undergo surgical removal without any remarkable consequences.
On the other hand, a group of only late-presenting 100 appendicitis patients will require more care due to life-threatening complications and bad general conditions.
For reasons that are quite complex but well-known, most Africans would rely on painkillers and some alternative medicines before seeking professional care as the last resort. Such behavior often makes a relatively simple condition get worse.
Inflammation of the appendix is more common in teens and young adults (adolescents) in their 20s when they consume a lot of junk food.
According to the Mayo Clinic, it’s rare to have an inflamed appendix in the very young and in old age. (5)
Healthcare professionals believe that appendicitis is caused by a wandering foreign object blocking the opening of your appendix, making it swell, collect bacteria, get inflamed, and then cause pain.
Whatever this object may be (fecal (stool) matter, an undigested piece of food, or even parasites in your intestine), bacteria will make use of the closed environment to fill the appendix with pus and cause increased pressure and symptoms.
Without immediate care, the most common complication of appendicitis is perforation - a hole through the inflamed appendix. (6)
Pain is the first thing that you feel following an inflammation of the appendix. (7)
If you ever feel this type of pain, it means that your appendix has been inflamed for at least 12-24 hours.
You should see your doctor or go to the emergency department of your local hospital as soon as possible to prevent complications.
Other general symptoms that usually appear after pain are: (5)
As the disease progresses, these symptoms may increase.
Based on your complaints your doctor will take your full medical history and ask about
On completion of your medical history, your doctor will perform a physical examination on you with a special focus on the pain in your abdomen.
 During the examination of your abdomen, your doctor may:
During the examination of your abdomen, your doctor may:
Other parts of your body are also examined including your chest, heart, kidneys, knee joints, etc.
Your doctor may also perform the following additional examinations:
Based on your medical history and physical examination findings, your doctor will most likely diagnose you with appendicitis.
To confirm the diagnosis, your doctor may then order the following laboratory tests:-
Diagnosis of appendicitis is simple due to characteristic complaint, so imaging tests are usually saved for complicated cases such as
The imaging tests may include:
Note that some of these tests may be hard to perform in many African healthcare settings because the equipment is not available, or the test is too expensive for the patient to afford.
That’s why many physicians rely on patient complaints and their clinical and diagnostic skills to make a diagnosis of appendicitis. (6)
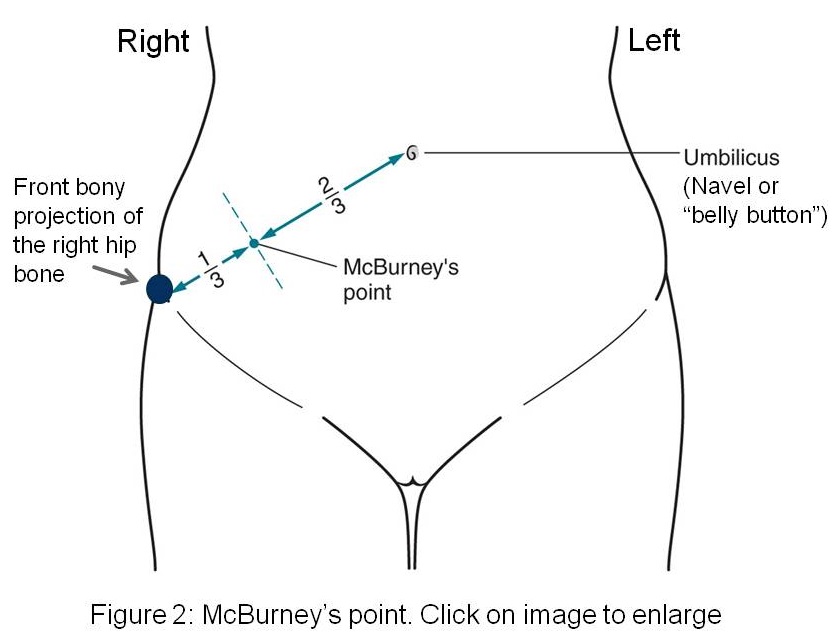
You can check yourself for appendicitis at home by doing a simple test:-
However, self-diagnosis is not advisable, as you may take unnecessary medications and delay seeking professional help.
It’s always better to see a doctor promptly whenever you suspect you may have the symptoms of appendicitis.
Many other disorders of the abdomen and pelvis may mimic the symptoms and clinical findings seen in patients with appendicitis.
Some of these include:(6)
The pain of period cramps may mimic that of appendicitis but there are a few pointers that may help you tell one condition from the other.
Let us look at some of these pointers:
Most women are aware that their menstrual period is cyclical and occurs every 28 days on an average. This is what can be referred to as periodicity.
Also, most women that have experienced period cramps expect it to happen 2-3 days before and after their period, reaching peak intensity after 24 hours.
On the contrary, the pain of appendicitis is sudden and is never regularly or irregularly associated with the mentrual period cycle.
Women with period cramps report feelings of diffuse dull pains in the lower pelvis. They also feel it in the low back, hip, or thigh.
Whereas the pain of appendicitis may start as a dull pain in the central upper abdomen and then moves to the right lower abdomen as a sharp pain.
The pain of appendicitis is often associated with general symptoms like fever, nausea, or vomiting, but such symptoms are absent in period cramps in the absence of pelvic inflammatroy disease (PID).
The most notable complication of untreated appendicitis is when the appendix bursts (rupture or perforates) and spreads its toxic infective content inside the abdominal peritoneum (a silk-like sac enclosing your abdominal organs).
This is a life-threatening condition known as peritonitis. and studies suggest that the average risk of this condition occuring after 36 hours of onset of symptoms is between 16 - 36%
If not treated promptly and adequately, the toxic content causing peritonitis may spread into your blood and eventually into all of your body causing a fatal condition known as toxemia or sepsis. So peritonitis following rupture of the inflamed appendix requires emergency care.
When the body tries to contain the infection resulting from a rupture of the appendix, it forms a pocket around the inflamed and ruptured appendix. This pocket is known as an abscess, and it contains pus or inflammatiory products.
An appendix abscess may also form as a complication of appendix surgery. This will be discussed more in a different article.
As with any abscess, an appendix abscess must be drained at a hospital.
At the time of drainage, your doctors will give you appropriate antibiotics treatment before you’re scheduled to get an urgent surgery to remove the abscess and appendix.
A delay in seeking medical care for an appendix abscess can lead to serious complications, including death.
The standard treatment of appendicitis is to remove it in a surgery called an appendectomy. (or appendicectomy)
This surgery is well-established and effective. It also doesn’t have a long-term impact on your life since the appendix is not known to play a critical role in the body.
How this surgery is performed and the complications that may arise, is the subject of a different article.
Although antibiotics can treat any bacterial infection, it’s always recommended to remove an inflammed appendix as the infection tends to recur making the appendix progressively weaker and more liable to burst causing complications.
In addition, antibiotic therapy can relieve pain and eradicate bacteria, but it may make the inflamed appendix stick to neighboring structures and the surgical option will be more difficult.
For recurrent appendicitis, surgery is a must.
1. What Is an Appendix, and What Does It Do? Everyday Health [Internet]. Last reviewed Sept. 22. 2022. [cited 2023 May 19]. Available from: https://www.everydayhealth.com/appendicitis/guide/appendix/
2. T Guan L, Liu Z, Pan G, Zhang B, Wu Y, Gan T, Ouyang G. The global, regional, and national burden of appendicitis in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. BMC Gastroenterol. 2023 Feb 22;23(1):44. doi: 10.1186/s12876-023-02678-7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9945388/
3. Ferris M, Quan S, Kaplan B, Molodecky N, Ball C, Chernoff G, Bhala N, et al. The Global Incidence of Appendicitis: A Systematic Review of Population-based Studies. Annals of Surgery 266(2):p 237-241, August 2017. | DOI: 10.1097/SLA.0000000000002188. Available from:
journals.lww.com//Global_Incidence_of_Appendicitis
4. Noudeh YJ, Sadigh N, Ahmadnia AY. Epidemiologic features, seasonal variations and false positive rate of acute appendicitis in Shahr-e-Rey, Tehran. Int J Surg. 2007 Apr;5(2):95-8. doi: 10.1016/j.ijsu.2006.03.009. Available from: https://pubmed.ncbi.nlm.nih.gov/17448972/
5. Appendicitis - Symptoms and causes - Mayo Clinic [Internet]. August 7,2021. [cited 2023 May 19]. Available from: https://www.mayoclinic.org/diseases-conditions/appendicitis/symptoms-causes/syc-20369543
6. Appendicitis: MedlinePlus. NIH National Library of Medicine. [Internet]. Last reviewed April 21, 2021. [cited 2023 May 19]. Available from: https://medlineplus.gov/ency/article/000256.htm
7. Appendicitis - Symptoms - NHS [Internet]. Last reviewed Oct. 21, 2022.[cited 2023 May 19]. Available from: https://www.nhs.uk/conditions/appendicitis/symptoms/
8. Afuwape OO, Ayandipo OO, Soneye O, and Fakoya A. Pattern of presentation and outcome of management of acute appendicitis: A 10-year experience. J Clin Sci. 2018 (15) 4, 171-175. DOI: 10.4103/jcls.jcls_105_17.
Published: July 6, 2023
© 2023. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content without alteration or modification and subject to attribution as to source.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.