
Colon cancer: Location representation
When Adeniran Chukwuemeka (not the real name) died one year ago, his family - unusual for an African family, was gracious to disclose his cause of death. It was colon cancer (also commonly referred to as bowel cancer).
‘Niran died, aged 62. He was a doctor and distinguished public health specialist.
His family felt that disclosing his cause of death will help to raise awareness about colon cancer in the community he grew up in and worked.
According to ‘Niran’s wife, her husband had been complaining of irregular stooling, occasional tummy pains and seeing blood in stool off and on for well over a year prior to his death.
“He believed he had hemorrhoids and considered his busy work-life schedule were to blame for his complaints”, said ‘Niran’s wife.
Even for a doctor, it never crossed ‘Niran’s mind that his complaints could indicate a more serious ailment. So, he never sought medical attention until it was too late.
By the time ‘Niran eventually visited his doctor to complain, he had started having more frequent and troublesome abdominal pain. The sighting of blood in stool were more consistent and sometimes continuous.
Eventually, ‘Niran was diagnosed with colon cancer for the first time three months prior to his death.
At the time Niran was taken to surgery, it was discovered that he had very advanced stage colon (lower bowel) cancer that had spread to involve many organs in his abdomen and his bones.
‘Niran’s wife said: “His doctor said he had stage IV colon cancer and surgery was suspended. Supportive medical treatment was substituted. He became poorly rapidly soon thereafter.”
“My husband’s doctor told me after his death, that ‘Niran could have been saved from bowel cancer if he had come up with his complaints several years ago”, said ‘Niran’s wife.
“I urge everyone, male or female, in mid-life stage with history of any bowel complaints to get a doctor’s checkup promptly and early”.
“Early detection could have saved my husband”, she said.
Colon cancer is a type of cancer that begins in the large intestine (colon). About 65% of colon cancers occur in the rectum/sigmoid colon area and 15% in the ascending colon (see illustration). The colon and its different parts form the final part of the digestive tract.
.jpg)
Image showing different parts of the colon. Any part can be affected by colon cancer, but the recto-sigmoid colon is affected most. Image credit: Mayo Clinic
In Sub-Sahara Africa, colon cancer is considered to be the 5th commonest cancer with an estimated incidence rate of 4.04 per 100 000 population (4.38 for men and 3.69 for women).1 This is very likely an under-estimation.
Colon cancer typically affects older adults, though it can occur at any age. It usually begins as a small, noncancerous (benign) growth of cells called polyps that form on the inside of the colon. Over time some of these polyps can become colon cancers.
Polyps may be small and produce few, if any, symptoms. For this reason, doctors recommend regular screening tests to help prevent colon cancer by identifying and removing polyps before they turn into cancer.
As in the case of ‘Niran, the symptoms of bowel cancer can often be subtle and don’t necessarily make you feel ill.
More than 90 per cent of people that are diagnosed with bowel cancer will have one or more of the following symptoms:
Most people with these symptoms may not have bowel cancer.
If you experience one of more of these symptoms and they persist for more than four weeks, you are best advised to visit your doctor.
The cause of colon cancer is not known. In general colon cancer like most other cancers start when healthy cells develop abnormal changes (mutation) in their DNA. A cell’s DNA contains a set of instructions that tells the cells what to do.
In colon cancer, tansformative mutation is believed to occur in non-cancerous small tissues (polyps) that grow inside the inner lining of the large bowel (colon). If not detected early and removed, the polyps will become cancerous, spread beyond the colon and may eventually be a cause of death.
While the exact cause of bowel cancer is unknown, there are a number of factors that can increase your risk, including:
If you experience one of more of the symptoms that may indicate colon cancer and they persist for more than four weeks, you are best advised to visit your doctor.
Your doctor will take a full history from you and may decide to:
It is recommended that you start colonoscopy from age 45 to 50 years and probably earlier if you have a family history of the condition. Thereafter, colonoscopy is recommended every 10 years.
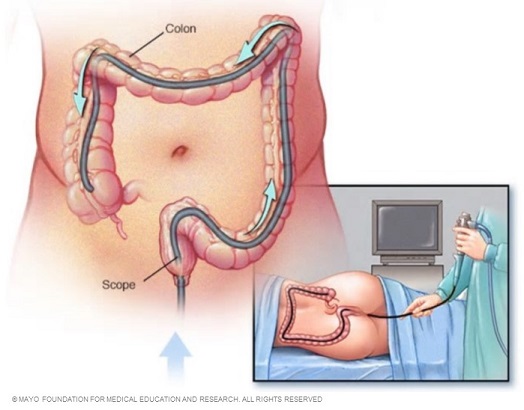
Colonoscopy: During a colonoscopy, the doctor inserts a colonoscope into your rectum to check for abnormalities in your entire colon. Image credit: Mayo Clinic.
If you've been diagnosed with colon cancer, your doctor may recommend tests to determine the extent (stage) of your cancer. Staging helps determine what treatments are most appropriate for you.
In many cases, the stage of your cancer may not be fully determined until after colon cancer surgery, but tests used in staging may include imaging procedures such as abdominal, pelvic and chest CT scans.
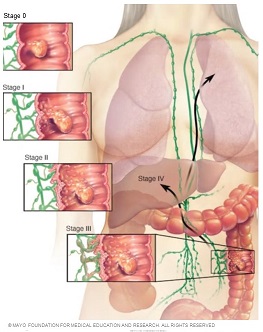
Colon cancer staging: At its earliest stage (stage 0), colon cancer is limited to the inner lining of your colon. As colon cancer progresses, it can grow through your colon and extend to nearby structures. The most advanced stage of colon cancer (stage IV) indicates cancer has spread to other areas of the body, such as the liver or lungs. Image credit: Mayo Clinic
The stages of colon cancer are indicated by Roman numerals that range from 0 to IV, with the lowest stages indicating cancer that is limited to the lining of the inside of the colon. By stage IV, the cancer is considered advanced and has spread (metastasized) to other areas of the body.
Treatment options offered for colon cancer varies with the location of the cancer, the stage of the disease and other co-existing medical conditions at time of diagnosis.
Generally, treatment for colon cancer usually involves surgery to remove the cancer. Other treatments, such as radiation therapy and chemotherapy, might also be recommended.
If your colon cancer is very small, your doctor may recommend a minimally invasive approach to surgery, such as:
If the cancer has grown into or through your colon, your surgeon may recommend any of the following surgeries depending on your particular situation:
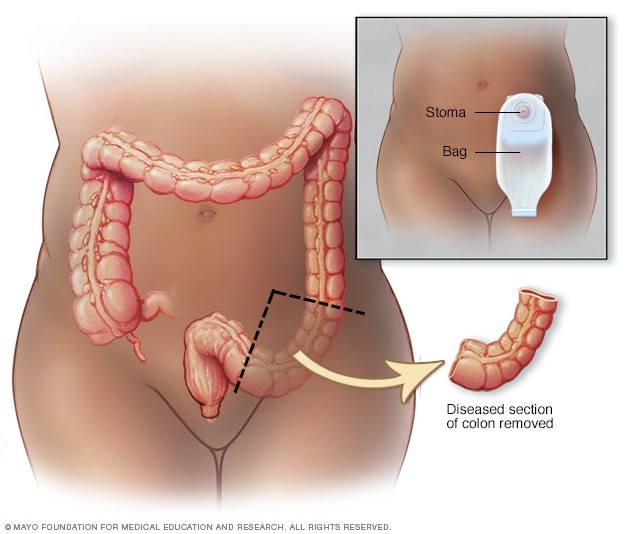
Partial colectomy. showing resected area of colon (sigmoid) containing the cancer along with margin of normal tissue on either side. sigmoi colon. When the free margins are not sewn back immediately, an ostomy is commonly created to serve as temporay evacuation for stool. Image credit: Mayo Clinic.
Sometimes the ostomy is only temporary, allowing your colon or rectum time to heal after surgery. In some cases, however, the colostomy may be permanent.
In addition to minimising risk factors for colon cancer, screening and early detection of pre-cancerous polyps is at the heart of prevention of colon cancer.
It is recommended that people with an average risk of colon cancer consider colon cancer screening around age 50. But those with an increased risk, such as those with a family history of colon cancer, should consider screening sooner.
Several screening options exist — each with its own benefits and drawbacks. Talk about your options with your doctor, and together you can decide which tests are appropriate for you.
You can take steps to reduce your risk of colon cancer by making changes in your everyday life. Take steps to:
Some medications have been found to reduce the risk of precancerous polyps or colon cancer. For instance, some evidence links a reduced risk of polyps and colon cancer to regular use of aspirin or aspirin-like drugs. But it's not clear what dose and what length of time would be needed to reduce the risk of colon cancer. Taking aspirin daily has some risks, including gastrointestinal bleeding and ulcers.
These options are generally reserved for people with a high risk of colon cancer. There isn't enough evidence to recommend these medications to people who have an average risk of colon cancer.
If you have an increased risk of colon cancer, discuss your risk factors with your doctor to determine whether preventive medications are safe for you.
Bottom line, colon (colorectal) cancer is the fifth commonest cancer in Sub-Saharan Africa. Men are slightly more at risk than women. Any age group from young adulthood may be affected, bit it is commonest from age 60 and above. Symptoms of colon cancer are non-specific and may be characterized by abdominal pain, blood in stool or rectal bleeding, fatigue, weakness and unexplained eight loss. Early presentation to your doctor helps early detection and better treatment options. Prevention of colon cancer calls for reduction of risk factors and yearly screening of at risk individuals.
Estimating the incidence of colorectal cancer in Sub–Saharan Africa: A systematic analysis
Eating Junk Food Can Raise Your Colon Cancer Risk
Eat African and drop your colon cancer risk
Be aware, thin size poop can be a clue to your colon cancer risk
Published: February 22, 2020
Updated: June 2, 2024.
© 2024, Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content freely for non-commercial purposes without alterations, adjustments or amendments and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.