By: Dr. Rahat Aisha Yasmeen, Freelance Health Writer and Datelinehealth Africa (DLHA) volunteer, with Editorial staff support.
.jpg) Key highlights
Key highlights
Diabetes is one of the most common lifestyle disorders that the world faces today and the Africa region tops the world in undiagnosed diabetes, according to a 2022 WHO analysis .
Currently, 24 million adults are living with diabetes in Africa. The figure is projected to rise by 129% to 55 million by 2045.
Factors such as lack of testing facilities and equipment, inadequate number of trained health personnel, poor access to health facilities and lack of awareness about diabetes are some of the barriers to diabetes management in Afrcan communities
The key risk factors and symptoms to look out for in the diagnosis of diabetes are well known. They include
Also well known are some of the diseases or complications associated with diabetes, such as
How uncontrolled or poorly controlled diabetes affects or impacts oral health to cause local diseases is the main focus of this report.
 Our healthy human mouth contains a variety of non-visible organisms (microflora) living in a balanced environment and reacting actively to stimulus and inflammatory agents.
Our healthy human mouth contains a variety of non-visible organisms (microflora) living in a balanced environment and reacting actively to stimulus and inflammatory agents.
As sugar level in blood rises especially in uncontrolled diabetes, so does the sugar content in saliva too.
The microflora in the mouth uses the high sugars as basic media to flourish and distort the normal threshold levels. This results in the formation of sticky plagues among other consequences.
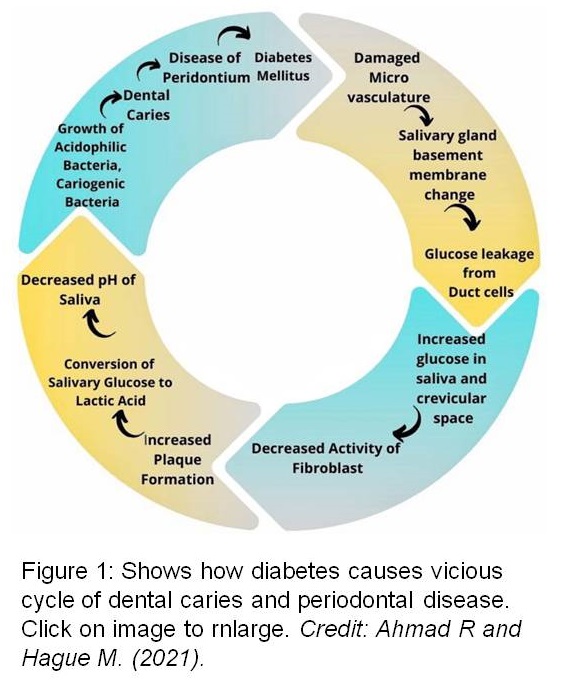
Sticky plaques that cover the teeth and gums host bacteria that in turn cause a vicious cycle of teeth decay, inflammation of gums and bad breath (figure 1).
If you have diabetes, the oral signs and complications to watch out for are summarised in figure 2 and include:
The periodic accumulation of fast growing sticky plaque around the tooth surface causes inflammation of the gums. As a result, the gums become red, swollen and painful. Swollen gums when aggravated cause bleeding due to poor oral hygiene and poor wound healing.
The high amount of sugars in saliva is converted into lactic acid by the bacteria growing in the sticky plagues. This acid lowers the acidity (pH) of saliva, which in turn acts on enamel of the teeth to damage them, thereby causing the formation of cavities or holes (dental caries) with high food lodgment.
People with uncontrolled diabetes with high glucose levels in the oral cavity also have sweet breath due to the presence of a chemical agent called ketones. In the presence of dry mouth, poor oral hygiene and coated tongue, the bacteria in the mouth act upon these sugary components to produce bad breath (halitosis).
Diabetes causes a reduction in salivary secretions along with change in composition of saliva and this leads to presence of rough tongue, chapped lips, dryness around the corners of the mouth and thicker saliva.
The presence of infections associated with dental caries such as dental abscess (pus filled cavity) or growth of opportunistic bacteria such as Candidiasis, Oral Lichen Planus etc. must be treated early to avoid further complications.
Candidiasis may appear as a long standing rash or white layer of sticky deposits (plaque) that are difficult to remove, on the moist inner lining (mucosa) of the gums and tongue. These infections are often painful and require the use of antibiotics, steroids and pain killers to treat.
Poorly controlled or uncontrolled diabetes contribute to changes in taste sensation or elevation of detection threshold. Nearly 1 in 20 diabetics have being shown to have sweet taste disorder, while 1 in 12 have a salt taste disorder. The cause of the taste disorder is complex and may be partly due to dry mouth and sensory (taste) nerve dysfunction.
The damage that occurs to sensory nerves in diabetic patients is called neuropathy in medical terms. This damage contributes to an increase in the taste threshold in the mouth. The taste dysfunction may also cause inability to maintain a good diet, which in turn leads to poor sugar control.
Also, the sensory nerve disorder seen in diabetic patients may produce a hot, burning or tingling sensation inside the mouth that is known as burning mouth syndrome.
Premature loosening of teeth, tooth pain and loss of bone around the teeth occur when initial signs and symptoms of diabetes are ignored. Loose teeth pose a high risk for infection or tooth fracture causing hindrance to eat food normally and therefore poor sugar control.
Oral complications are often the first indicators of diabetes in undetected cases.
 Dentists are able to note minute and early changes in the oral cavity that indicate the presence of diabetes. Hence, you will be better off to take the following steps in order to ensure that you can identity and prevent several life-threatening oral diseases before they cause any damage.
Dentists are able to note minute and early changes in the oral cavity that indicate the presence of diabetes. Hence, you will be better off to take the following steps in order to ensure that you can identity and prevent several life-threatening oral diseases before they cause any damage.
Evidence point to poor oral hygiene as a risk factor for various heart and other systemic diseases. So, it is recommended that you undertake routine oral check up at regular intervals of six months. Preventive oral care (prophylaxis) maintained with proper brushing techniques helps reduce major complications. Early correction of teeth alignment, restoration of dental cavities and replacement of missing teeth boosts confidence for that desirable pearly white smile!
It is important that you maintain a good diet that include more fiber, protein and optimal carbohydrates and fats as these play significant roles in maintaining sugar levels in body.
Foods having high fiber such as fresh fruits and vegetables help to neutralize the action of acids and enzymes on teeth, thereby protecting the enamel layer around the teeth.
Calcium enriched foods help replenish mineral deposits in the body and also improves salivary flow. Cheese, milk, plain yogurt, and other dairy products are recommended, while sugary foods such as sodas, juices, cakes and rice should be avoided.
If you smoke or use of nicotine, it is better that you stop doing so.
Smoking worsens the symptoms of dry mouth and the risk of oral cancer. The chewing of tobacco is one of the highest causative factors for cancer of the lip, palate and oral mucosa.
According to GLOBOCAN 2012, oral cancer related deaths make up the twelfth and sixteenth most common cause of cancer mortality globally amongst males and females, respectively. In Nigeria, oral cancer has been estimated to account for about 1146 new cases, with an estimated mortality of 764 cases annually in 2012.
Alcohol consumption is also another causative factor for cancer and poor wound healing among others. So it is best for you to abstain from or moderate alcohol use in the interest of good oral care.
A combination of exercise, body fat control and good sleep is necessary for you to live a healthy and active lifestyle.
If you have type 2 diabetes, you are advised to undertake at least 150 minutes of moderate-intensity aerobic exercise and at least 90 minutes of vigorous aerobic exercise per week. This also helps you to reduce the risk of cardiovascular complications.
Since pregnancy induced gum and bone infections in the mouth due to varying hormonal levels in the body are common, it is important that you see your dentist before planning a pregnancy and during the pregnancy to address any issues.
Also be mindful that women may suffer from undetected diabetes during pregnancy (gestational diabetes). This can worsen gum and bone infections in the mouth and adds to the need to seek dental care during pregnancy.
Ask your doctor or nurse if you need to take nutritional supplements as these can help pregnant diabetic women to achieve better immunity and good oral hygiene.
Diabetes is a systemic disorder and must be treated with appropriate preventive and palliative care. You should be vigilant to notice early signs and symptoms associated with this disease especially in the oral cavity, where they can be more easily detected. Early detection is the best treatment!
World Health Organization. African region tops world in undiagnosed diabetes: WHO analysis. November 14, 2022. Accessed June 12, 2023.
US Centers for Disease Control and Prevention. Diabetes and Oral Health. Last updated December 20, 2022. Accessed June 12 2023.
Simpa Z. Management of type two diabetes in Nigeria. Datelinehealth Africa. June 1, 2023. Accessed June 12, 2023.
NIH. National Institute of Dental and Craniofacial Research. Burning Mouth Syndrome. Last updated September 2022. Accessed June 12 2023.
Ahmad R. and Haque M. (2021). R E V I E W Article Oral Health Messiers: Diabetes Mellitus Relevance. Diabetes Metab Syndr Obes. 2021 Jul 1;14:3001-3015. doi: 10.2147/DMSO.S318972.
Rohani B. Oral manifestations in patients with diabetes mellitus. World J Diabetes. 2019 Sep 15;10(9):485-489. doi: 10.4239/wjd.v10.i9.485.
Omitola OG, Soyele OO, Sigbeku O, Okoh D, Akinshipo AO, Butali A, Adeola HA. A multi-centre evaluation of oral cancer in Southern and Western Nigeria: an African oral pathology research consortium initiative. Pan Afr Med J. 2017 Sep 22;28:64. doi: 10.11604/pamj.2017.28.64.13089. PMID: 29599879; PMCID: PMC5873219.
Al-Maskari AY, Al-Maskari MY, Al-Sudairy S. Oral Manifestations and Complications of Diabetes Mellitus: A review. Sultan Qaboos Univ Med J. 2011 May;11(2):179-86. Epub 2011 May 15. PMID: 21969888; PMCID: PMC3121021.
 Management of type two diabetes in Nigeria.
Management of type two diabetes in Nigeria.
The right ways to maintain your dental health
Dental care in Africa: Challenges and solutions
Published: June 23, 2023
© 2023. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content without alteration or modification and subject to attribution as to source.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.