Glaucoma in Africa, especially in Sub-Saharan Africa, is a public health problem and the second-leading cause of blindness.
By: Elizabeth Obigwe. Datelinehealth Africa Volunteer Freelance Writer, with editorial support from The DLHA Team

The eyes produce a fluid known as aqueous humour in a structure called the ciliary body. This is different from tears that lubricate the eye surface. Usually, as this fluid is produced, a near equal amount of the fluid flows out through an area of the eyeball called the drainage angle (See figure 1).
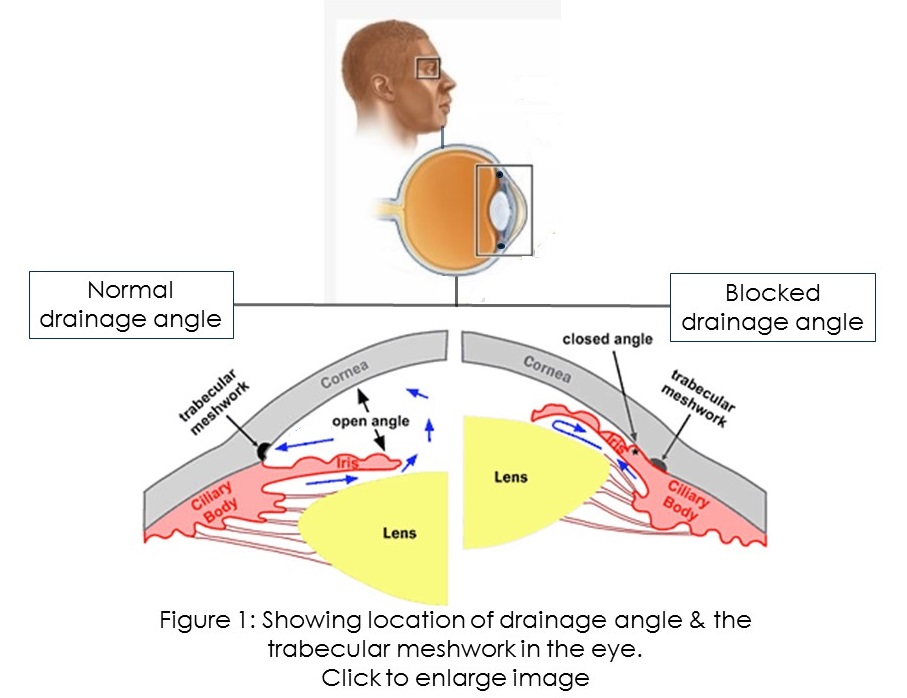 The drainage angle is the junction between the iris (the coloured part of the eye) and the sclera (the white part of the eye). At this angle, there is a structure called the trabecular meshwork. It is the outer part of the channel from which aqueous humour drains out. This drainage process helps to maintain the pressure within the eyes, that is, the intraocular pressure (IOP). Normal IOP is between 10 to 21 mm Hg, and glaucoma occurs when the IOP rises consistently above 21 mm Hg.
The drainage angle is the junction between the iris (the coloured part of the eye) and the sclera (the white part of the eye). At this angle, there is a structure called the trabecular meshwork. It is the outer part of the channel from which aqueous humour drains out. This drainage process helps to maintain the pressure within the eyes, that is, the intraocular pressure (IOP). Normal IOP is between 10 to 21 mm Hg, and glaucoma occurs when the IOP rises consistently above 21 mm Hg.
If the drainage angle stops functioning properly and aqueous humour builds up in the eyes, the intraocular pressure will rise, damaging the optic nerve. Many studies on glaucoma patients in different African countries point to median IOP in the range of 15 – 50 mm Hg.
The optic nerve is responsible for carrying messages from the eye to the brain. Damage to it due to raised IOP will affect your vision. This condition is called glaucoma.
Glaucoma in Africa, especially in Sub-Saharan Africa, is a public health problem and the second-leading cause of blindness. It tends to have an earlier onset and is more aggressive in its course.
This disease and how it affects vision will be discussed in the coming sections.
Glaucoma is a group of eye conditions that affect the optic nerve, causing continuous damage and eventually leading to blindness.
The damage this disease causes is irreversible. But there are treatment options that doctors use to manage the condition to prevent further progression.
In its early stage, glaucoma is asymptomatic (that is, you might not notice any symptoms until the condition gets worse). Hence, it is called “the silent thief of vision.”
Although glaucoma is often a result of high eye pressure, people with normal eye pressure may also suffer from this condition. And it can affect either one or both eyes. Also, this disease is most common in older adults above 60 years, but it can affect people of any age.
Glaucoma is one of the leading causes of vision impairment according to the World Health Organization (WHO). The organization also reports that 7.7 million cases of glaucoma globally could have been prevented or are yet to be addressed.
 In Africa, Glaucoma accounts for 15% of blindness and Africa is the region with the highest prevalence of blindness compared to other world regions. Although there is no known reason for the high prevalence of Glaucoma in Africa, poor awareness plays a role in it.
In Africa, Glaucoma accounts for 15% of blindness and Africa is the region with the highest prevalence of blindness compared to other world regions. Although there is no known reason for the high prevalence of Glaucoma in Africa, poor awareness plays a role in it.
Also, a 2022 study revealed that glaucoma is the leading cause of irreversible blindness. And it currently affects about 3.5% of people between the ages of 40 to 80. The study also predicted that by 2040, the disease will affect nearly 112 million people.
The International Agency for the Prevention of Blindness (IAPB) reports that about 6 million have glaucoma and up to half a million of them are already blind in Africa. Early detection is vital in managing glaucoma. However, about 50% of people living with glaucoma in underdeveloped countries are unaware that they have this condition.
Therefore, there is a need for more people to learn about this condition, the risk factors and the importance of early detection.
There are many types of glaucoma, but it is majorly divided into these five groups:
In open-angle glaucoma, there is no obstruction to the trabecular mesh. But, other parts of the drainage channel do not function properly. This causes a gradual buildup of eye pressure.
One of the most common types of open-angle glaucoma is normal tension glaucoma. In normal-tension glaucoma, there is no increase in intraocular pressure, but the optic nerve gets damaged for some other reason. Some scientists suggest that the damage might be due to extreme sensitivity or insufficient blood supply to the optic nerve.
Open-angle glaucoma (also called wide-angle glaucoma) is the most common type of glaucoma in Africa.
An educational article on Primary Open Angle Glaucoma (POAG) in Sub-Saharan Africa published in 2013 cited a population-based survey in rural East Africa that indicated a prevalence of 3.1% for POAG. Hospital based surveys like the one in Ghana and Nigeria however reported prevalence as high as 44.2% and 11.5% respectively for POAG.
This occurs when the drainage angle suddenly blocks and it is also called acute angle closure glaucoma. The blockage sometimes occurs when the iris bulges and closes the angle. The result is a rapid increase in eye pressure. This type of glaucoma manifests faster than the open-angle and is regarded as a medical emergency. Doctors also call it narrow-angle glaucoma.
In primary glaucoma, there is no pre-existing disease that affects eye pressure. The damage to the optic nerve here is either due to increased pressure caused by poor drainage or other reasons like limited blood supply to the optic nerve. Primary glaucoma can be categorized into primary open-angle glaucoma (POAG) and primary angle-closure glaucoma (PACG).
This occurs when a health condition increases the pressure in your eye. This condition might be one that affects the eye like cataracts or one that affects other parts of the body like diabetes.
For example, if you have a condition called ocular ischemia, new blood vessels will form over your iris and the drainage angle. This will result in a type of secondary glaucoma called neovascular glaucoma.
Other causes of kinds of secondary glaucoma are also known and they include trauma, inflammation and many more that are beyond the scope of this article.
Some babies are born with glaucoma or it may develop during the first few years after birth. This may occur if the drainage does not develop properly or something blocks it. An underlying medical condition may also be the cause of congenital glaucoma. Other names for it are developmental, infantile or pediatric glaucoma.
Generally, glaucoma occurs when there is damage to the optic nerve. This damage causes blind spots to develop in your vision.
For some glaucoma cases, damage to the optic nerve is due to increased eye pressure.
However, there are other cases where there is no increase in eye pressure. Scientists are yet to discover what causes the damage in these cases.
Glaucoma symptoms vary depending on the type.
 Symptoms of Open-Angle Glaucoma include:
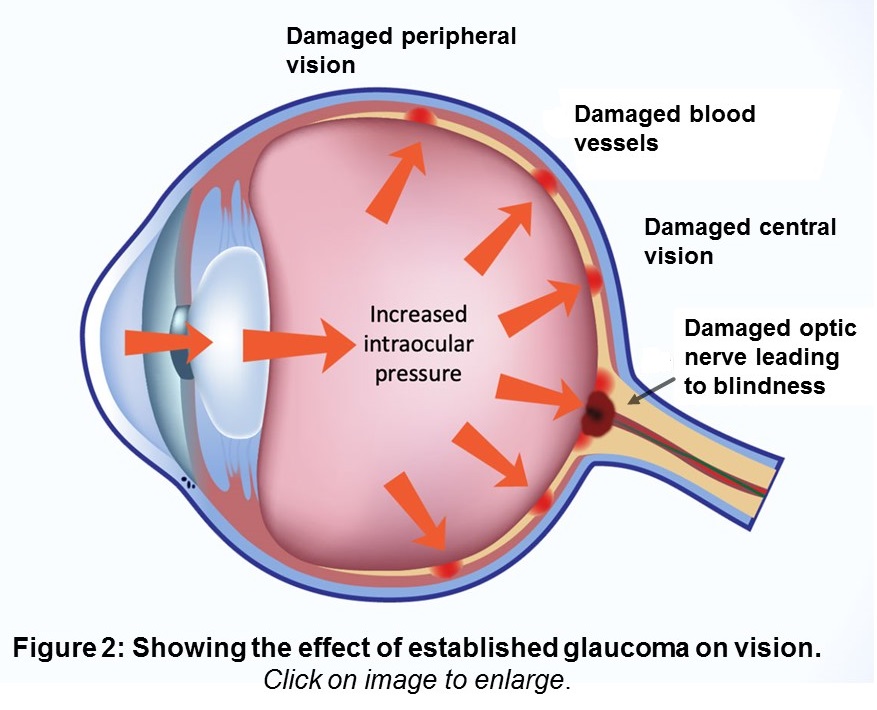
Symptoms of Open-Angle Glaucoma include:See figure 2 for eye structures that are damaged in glaucoma.
Below are some factors that can increase your risk of developing glaucoma.
Glaucoma is hereditary. Hence, if a member of your family has glaucoma, it increases your chances of suffering from it too. However, the chances vary depending on the degree of closeness with the family member. If the person is a first-degree relative (sibling or parent), the chances are higher than if the person is a distant relative.
The problem with family history is that many glaucoma cases are undiagnosed. Hence, a person with potential risk might not know that they are at risk because the family member who is suffering it already has not been diagnosed.
POAG is more common among Blacks and Hispanics. They also have severe manifestations and a higher risk of blindness. The Inuit, Chinese, Asian Indians, and Southeast Asians are more likely to suffer PACG. Generally, people in developing countries have a higher prevalence of glaucoma and a high risk of blindness.
The National Eye Institute reports that people who are Hispanic/Latino have higher chances of suffering glaucoma once they get to 60 years. While the risk age for African Americans is 40 years and older. A study on Glaucoma in Africa also showed a similar approximate age of onset value of 40 years. The risk continues to increase as Africans and others get older.
Research shows that myopia (shortsightedness) is a risk factor for glaucoma. The risk of developing glaucoma increases with an increase in the degree of myopia. Other eye problems like chronic inflammation and physical injury or trauma to the eye increase eye pressure, thus increasing the risk of glaucoma.
People who have health records of diabetes, systemic hypertension, vasospasm, and acute hypotension are at risk of suffering from glaucoma.
Prolonged use of certain drugs such as corticosteroids predisposes you to secondary glaucoma.
Continuous exposure to activities that increase or fluctuate the intraocular pressure puts you at greater risk of suffering glaucoma. Some of these activities are;
There is no known way to prevent glaucoma. However, checking your eyes regularly can help you detect it on time and prevent it from worsening. Doctors recommend annual routine checkups. This is especially important for people who have higher risks of developing the condition.
Unfortunately, many people who are at risk of glaucoma in Africa do not go for these routine checkups.
Eye doctors (ophthalmologists) use this test to measure the pressure of the eye.
First, the doctor will numb the eye with an anaesthetic (i.e., a fluid that induces insensitivity to pain). Next, he will put dye in the eye before shining light on it. The doctor then touches the eye with a tonometer to measure the pressure.
Alternatively, the doctor may use a different instrument that uses a puff of air instead of direct contact to check the pressure.
Ophthalmologists use this procedure to check if the angle between the cornea and the iris is functioning normally. This is also a painless procedure as the doctor will first numb the eye with an eye drop. Then he will place a special contact lens with mirrors on the eye. He will then use light to examine the drainage angle to see whether it is open or closed
Ophthalmologists use this procedure to check if glaucoma has affected any area of your vision, especially the side vision. The doctor will show you a sequence of light spots and you are to indicate the ones you see. The ones you cannot see may be an indication of the area glaucoma has affected. This procedure is also called the visual field test.
Pachymetry is a procedure where the doctor measures the thickness of the cornea. People with thin cornea are more likely to develop glaucoma. After numbing the eye, the doctor will touch the surface of the cornea with a small probe of the pachymeter. Then using ultrasound waves, the probe will read the thickness of the eye.
5. Examining the Optic Disc and Cup
 Because glaucoma usually affects the optic nerve, the doctor may want to examine the optic disc or optic disk and the optic cup. The optic disc is a raised impression at the back of the eye where the optic nerve fibres carrying information from inside the eye to the brain and the vessels supplying blood to the innermost layer of the eye pass through the eyeball.
Because glaucoma usually affects the optic nerve, the doctor may want to examine the optic disc or optic disk and the optic cup. The optic disc is a raised impression at the back of the eye where the optic nerve fibres carrying information from inside the eye to the brain and the vessels supplying blood to the innermost layer of the eye pass through the eyeball.
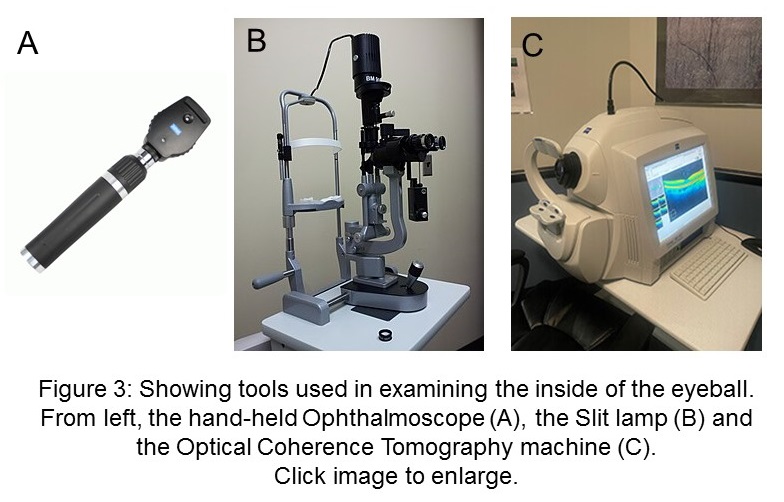
The doctor will first put an eye drop to make the pupil larger and then examine it using either of these tools and methods (see figure 3):
The appearances of a normal optic disc, nerve and cup is compared with that of an unhealthy optic disc, nerve and cup in glaucoma (see figure 4).
Notice that the optic cup enlarges in glaucoma as more optic nerve fibres are damaged. Usually an optic cup to disc ratio above 60% is indicative of glaucoma.
There is no cure for the glaucoma and damages done before diagnosis cannot cannot be reversed. This is why it is important to check your eyes regularly and see a doctor as soon as possible if you feel any discomfort in your eye.
The treatment or management process of glaucoma helps to prevent further damage and eventual vision loss.
There are different treatment options available for the different types of glaucoma. Your doctor might use a combination of these options.
Usually, the management of glaucoma patients is individualized and takes into consideration, the presenting IOP, the age of the patient, the severity of damage and the socioeconomic status of the patient.
Some of the management options are discussed below:
This can be either an eye drop or an oral medication.
Eye Drop: Using eye drop is the most common treatment option for glaucoma. It helps to reduce the production of fluid while improving its flow out of the eyes. Thus, reducing intraocular pressure.
There are several types of eye drops that are used in the medical treatment of glaucoma. Your eye doctor will discuss the best option for your clinical profile at any given time.
Irritation, eye redness, blurry vision, stinging and headache are some of the possible side effects of eye drops.
Oral Medication: Oral medication works just like the eye drop. It slows down fluid production and improves drainage.
This process involves using a laser (a strong beam of light) to clear up the drainage channel. The doctor first uses drops to numb the eye. And with a special lens, he aims the beam into the eyes. The beam then tries to improve fluid drainage.
There are different types of laser treatments. The one called trabeculoplasty is used to treat open-angle glaucoma.
During treatment, the laser may scratch the cornea or make it dry. This may be painful, but the pain does not last long. It goes away as the cornea heals.
There are different types of surgery for treating glaucoma. Usually, a doctor recommends surgery after medicine and laser options do not improve the condition.
Trabeculectomy: This surgery is mostly for open-angle glaucoma. The surgeon makes a tiny pathway in the eye through which extra fluid leaves the eye, thus reducing the pressure. It is also called filtering surgery.
Minimal Invasive Glaucoma Surgery (MIGS): MIGS is a new method that uses a milder approach and has fewer risks and side effects. There are different types of MIGS. Your doctor will decide the best option for you.
Glaucoma Implant Surgery: This is an alternative to trabeculectomy. In this case, the doctor inserts a silicone tube through the front of the eye so that it drains excess fluid. This option can treat different types of glaucoma including neovascular and congenital glaucoma. It is also more effective for people who have had previous eye surgeries.
 More and more people with glaucoma in Africa are losing their sight due to late or no diagnosis. Currently, scientists have not discovered the root cause of the disease. And the treatment options available can only hinder further progression but cannot reverse previous damage.
More and more people with glaucoma in Africa are losing their sight due to late or no diagnosis. Currently, scientists have not discovered the root cause of the disease. And the treatment options available can only hinder further progression but cannot reverse previous damage.
Hence, it is important for individuals to take steps to protect their eye health and reduce their risk of developing glaucoma. This includes maintaining a healthy lifestyle, avoiding smoking and excessive alcohol consumption, wearing protective eyewear when necessary, and monitoring any changes in their vision or eye health.
Also, public health managers at different levels of government need to continuously raise awareness within the community about glaucoma and implement cost-efficient policies and programs that will motivate Africans to present for regular eye check up in public and private health facilities for the early detection and management of the condition.
Related: Priority eye diseases in Africa (Slideshow)
Published: April 6, 2023
© 2023. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content without alteration or modification and subject to attribution as to source.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.