By: Elizabeth Obigwe. Datelinehealth Africa Volunteer Freelance Writer, with editorial support from The DLHA Team

Image of an African mother backing a toddler with flies perching on his eyes and other parts of his face
The front part of the eye is covered with two kinds of thin, transparent tissue layers; the cornea and the conjunctiva.
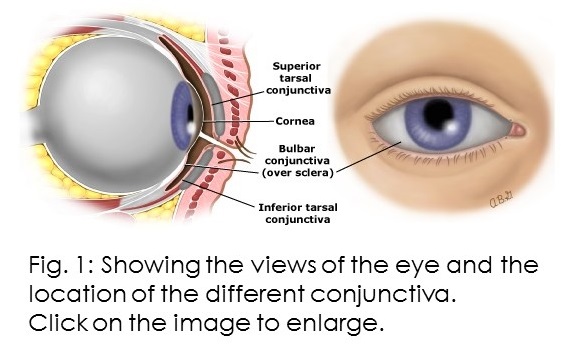 The cornea is the layer that lays over the Iris and pupil (the dark part of the eyes). While the conjunctiva is the layer overlying the sclera (the white part of the eyes) and which also extends into the inner part of the eyelids.
The cornea is the layer that lays over the Iris and pupil (the dark part of the eyes). While the conjunctiva is the layer overlying the sclera (the white part of the eyes) and which also extends into the inner part of the eyelids.
The conjunctiva which covers the white part of the eye is called the bulbar or ocular conjunctiva while the part covering the inner part of the eyelid is called the palpebral or tarsal conjunctiva.
At its early stage, trachoma disease begins with inflammation of the tarsal conjunctiva which then spreads to the ocular conjunctiva. This inflammation later develops into scarring of the conjunctiva and eventual corneal complications.
Trachoma is an infectious eye disease caused by a bacterium that affects both eyes. It first manifests as conjunctivitis (inflammation of the conjunctiva) which causes redness of the eye. This phase is also marked by mild itching of the eyes and eye discharge. The disease later progresses to corneal complications and irreversible vision loss. Early diagnosis and treatment can prevent the condition from worsening and save the patient’s eyesight.
The infection occurs in episodes which means that a person who gets infected might recover but is reinfected again. Doctors think that it is the recurrence of this infection that leads to the more complex stage of scarring and blinding complications.
This explains why the early stage of the infection is more common in younger children (below 5 years) and the later stage is more common in adults between the ages of 30 to 40. Generally, it takes years for trachoma to cause blindness but it might take a shorter time for some people.
Trachoma is a Neglected Tropical Disease (NTD) and the leading infectious cause of blindness globally. It is also the second leading cause of blindness in Africa (coming after cataracts, it is as much of a public health concern as glaucoma).
Trachoma affects mostly poor and underdeveloped countries, particularly rural areas. According to the World Health Organization (WHO), this disease is responsible for the visual impairment of about 1.9 million people and it causes about 1.4% of all blindness worldwide. Also, 2022 data from the WHO revealed that about 125 million people live in trachoma-endemic areas and are at risk of contracting it.
Trachoma occurs when a bacterium, Chlamydia trachomatis infects the conjunctiva — usually the tarsal conjunctiva. The infection results in a type of inflammation called follicular conjunctivitis and the signs are more severe on the upper eyelid than on the lower one.
The disease is transmitted through direct and indirect contact with the discharge from the eyes or nose of an infected person. Kids are more likely to have close contact with one another and rub their eyes with their hands. Hence, they have a higher chance of contracting the infection.
Trachoma is a progressive disease that continues to worsen in affected individuals if left untreated. Largely, the manifestation of this disease is grouped into two phases. The first is the early or active trachoma which is characterized by follicular or severe inflammation. The second phase is the late-stage or cicatricial phase which is characterized by scarring and vision-threatening complications.
However, the World Health Organization provided a simplified system for assessing trachoma. This system is made up of 5 stages that doctors observe with the help of a magnifier.
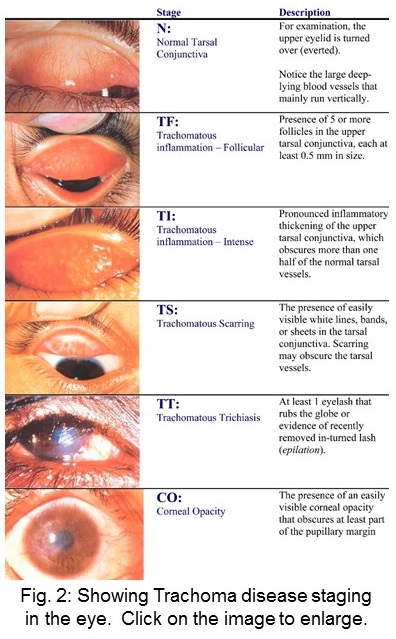 Stage 1: Follicular Trachoma (TF) - The follicular stage of the infection is indicated by the presence of five or more follicles in the centre of the upper tarsal conjunctiva. Each molecule must be at least 0.5mm in diameter. Usually, these follicles are round lumps or spots that are paler than the conjunctiva.
Stage 1: Follicular Trachoma (TF) - The follicular stage of the infection is indicated by the presence of five or more follicles in the centre of the upper tarsal conjunctiva. Each molecule must be at least 0.5mm in diameter. Usually, these follicles are round lumps or spots that are paler than the conjunctiva.
Stage 2: Trachomatous Inflammation-Intense (TI) - This is regarded as the most infectious stage of trachoma. At this stage, the surface of the inner eyelid becomes obviously inflamed and thick. More than half of the upper tarsal conjunctiva and the large deep vessels of the same area are not visible because the inflammation makes it hard to see.
Stage 3: Trachomatous Scarring (TS) - Recurrence of the infection can lead to scarring of the inner eyelid. These scars are seen as white lines, bands or sheets (fibrosis). Scarring can also conceal the blood vessels of the upper tarsal but your doctor will examine it carefully to distinguish it from TI. At this stage, the eyelid may become distorted and turn inward. A condition called entropion.
Stage 4: Trichiasis (TT) - This is the in-turning of the eyelashes. As the eyelid continues to deform, at least one of the eyelashes also starts to turn inward and rub/scratch the cornea. Vision can be restored at this stage if the doctor notices it on time.
Stage 5: Corneal Opacity (CO) - The cornea becomes scarred and inflamed so much that it becomes cloudy. This cloud appearance eventually covers part of the pupil margin resulting in blurred vision.
Living in or visiting an endemic area exposes you to the infection. But other factors like age, gender, overcrowding, poor sanitation, flies, etc. increase your risk of infection.
The manifestation of trachoma disease is greatly influenced by age. Pre-school children who are younger than five years are at greater risk of contracting the active disease. This is likely because they are more prone to coming in contact with their infected counterparts than adults who have more controlled interaction. Children make up 60% of the affected population in an endemic region. For adults, conjunctival scarring is more common among them. This shows that the disease has a cumulative nature.
Among kids, both genders have equal chances of suffering from trachoma. However, among adults, women are more likely to suffer from trichiasis and vision loss. This is probably because they are likely to spend more time caring for infected kids. Doctors say that when adults contract trachoma, the early infection episodes are probably very short which is why adults are hardly diagnosed with active trachoma.
Poor sanitation, lack of proper hygiene and inadequate water supply increase the spread of the disease. In 2021, the World Health Organization released a strategy on water, sanitation and hygiene (WASH) as part of the effort towards managing neglected tropical diseases like trachoma.
Trachoma disease is often found in clusters in endemic regions. Either within families or villages. This is due to the close interaction of the people. Overcrowding increases the likelihood of contact with infected persons thereby increasing the chances of infection.
Eye-seeking flies play a role in transmitting the infection from one person to another by feeding on the secretion from the eyes. Hence, these flies are common in regions where trachoma is prevalent, an example of such a fly is Musca Sorbens. These flies breed in human faeces. So areas that lack toilets or latrines are often prone to increased risk of trachoma.
A 2015 study revealed that children who sleep in unventilated rooms with cooking fires are at greater risk of severe trachoma. According to the study, cooking fires can release pollutants into the air and the pollutant can trigger inflammation, thereby worsening the infection.
These include:
If your eyes feel itchy or irritated, or if there's discharge coming out, it's important to contact a doctor immediately. This is especially crucial if you live in or have recently visited an area where trachoma is widespread. It is important that you get treatment quickly to prevent it from getting worse.
To diagnose trachoma, your eye doctor (ophthalmologist) will obtain a good history from you regarding the onset, course and other diverse information about your living conditions. An eye exam will then be performed and some laboratory tests may be requested.
The eye examination will involve the use of a tool that consists of a light source and simple glass magnifier. The eye examination will reveal if;
For the laboratory test, the eye doctor will numb your eye and swab the surface to take a sample. He will then go on to test if trachoma is the cause of the infection.
Yes, you can prevent trachoma. Controlling transmission is key in trachoma prevention.
Since the disease is communicable but not hereditary, you can prevent it by taking steps not to catch the infection or be reinfected.
If you live in an area with cases of trachoma, you and your family need to get screened to ensure that you have not already contracted the disease. If you are free, endeavour to maintain personal hygiene and proper waste management.
Also, the government and well-meaning organizations should provide clean water sources for residents of areas affected by trachoma.
To tackle trachoma with the right treatment methods, the World Health Organization developed a treatment strategy known as SAFE. The letters stand for Surgery, Antibiotics, Facial Cleanliness and Environmental Improvement.
Surgery is the first line of action in the treatment of patients at risk of blindness. It is done to reverse the eyelashes that have turned inward. This lid surgery is not complicated and a doctor can do it in a health or community centre. This procedure helps to stop the pain in the eye by preventing further scarring by the eyelashes. However, it does not reverse previous scars or restore sight.
The WHO recommends two types of antibiotics (azithromycin and tetracycline eye ointment) for the treatment of active trachoma. Your doctor will administer them as needed.
Children with dirty faces are more likely to transmit or get infected with trachoma. Eye-seeking flies are more attracted to dirty faces and they will sit on the discharge from the eyes and nose of an infected person and transfer the infection to another. Also, rubbing the sore eyes with hands, clothes, bedsheet or mother’s shawl can foster the spread of trachoma chlamydia.
Hence, it is important to educate people on the need to maintain facial cleanliness and avoid frequent touching of their faces. Also, clean water should be provided in affected areas to encourage face washing.
Environmental improvement is an important part of trachoma disease control that involves not only individuals but government sectors and NGOs. A dirty environment favours trachoma and many affected areas are dirty due to insufficient basic infrastructure for water, sanitation, and waste disposal. For proper control and elimination of the disease, these infrastructures should be made available. Otherwise, people may be reinfected even after treatment with antibiotics.
Africa, Central and South America, Asia, Australia and the Middle East are the key regions that are affected by this endemic disease with Africa being the most affected. Initially, 57 countries were marked as trachoma-endemic areas globally. In Africa, up to 33 countries were classified as trachoma-endemic regions (See Table).
Table showing list of Trachoma endemic Africa countries. Click on image to enlarge
As of 5 October 2022, the WHO has validated that 15 out of the 57 countries have successfully eliminated trachoma disease while 42 remain to achieve the same. These 15 countries are; Cambodia, China, Gambia, Islamic Republic of Iran, Lao People’s Democratic Republic, Ghana, Malawi, Mexico, Morocco, Togo Myanmar, Nepal, Oman, Saudi Arabia and Vanuatu.
So far, Benin, Gambia, Ghana, Mali, Malawi, Morocco and Togo are the only countries in Africa that have WHO’s validation as being trachoma free. Hence, they are the only African countries that have met the WHO’s goal of eliminating trachoma by May 16, 2023.
Nigeria is one of the countries that is yet to meet this goal. A study revealed that its inability to meet the goal was due to long-term negligence and lack of cooperation of different sectors. Trachoma is a Neglected Tropical Disease, so neglecting it might be part of the reason other African countries are yet to overcome it too.
Morocco on the other hand shared an insight into how they managed to eliminate the disease. Some of the elements that facilitated their success are;
Africa has made significant progress in controlling trachoma disease. However, as a leading region in the prevalence of the disease, it needs to do more in order to achieve the goal of eliminating the disease. Regions that have neglected trachoma should wake up and reignite campaigns against this disease. They should work with the WHO’s 2021-2023 road map for ending the neglect to attain the Sustainable Development Goals to achieve measurable results.
Also, efforts to address the social and environmental determinants of trachoma, such as poverty, lack of education, and poor sanitation, must be prioritized to ensure sustainable progress in trachoma elimination.
The different authorities and stakeholders with responsibility for public health should offer maximum cooperation to help save people from preventable blindness.
1. Bejiga A, Alemayehu W. Prevalence of trachoma and its determinants in Dalocha District, Central Ethiopia. Ophthalmic Epidemiology. 2001;8(2-3):119–25. doi: 10.1076/opep.8.2.119.4168. (Abstract).
2. Burton MJ. Trachoma: An overview. British Medical Bulletin. 2007;84(1):99–116. https://doi.org/10.1093/bmb/ldm034
3. Hammou J, Obtel M, Razine R, Berraho A, Belmekki M. Elimination of trachoma from Morocco: A historical review. Eastern Mediterranean Health Journal. 2020;26(6):713–9. doi: 10.26719/emhj.19.014.
4. Carter Cemter. Implementing the SAFE strategy for Trachoma Control. (PDF). Accessed, April 13, 2023.
5. Mohammadpour M, Abrishami M, Masoumi A, Hashemi H. Trachoma:Past, present and future. Journal of Current Ophthalmology. 2016;28(4):165–9. doi: 10.1016/j.joco.2016.08.011.
6. Nasir MA, Elsawy F, Omar A, Haque SO, Nadir R. Eliminating trachoma by 2020: Assessing progress in Nigeria. Cureus. 2020; Jul 29;12(7):e9450. doi: 10.7759/cureus.9450.
7. Thylefors B, Dawson CR, Jones BR, West SK, Taylor HR. A simple system for the assessment of trachoma and its complications. Bulletin of the World Health Organization. U.S. National Library of Medicine; 1987. Redirects to PDF page.
8. National Institute of Health, National Eye Institute.: Trachoma risk tied to sleeping near cooking fires, lack of ventilation. Accessed, April 12, 2023.
9. Trachoma - Sub-Saharan Africa. American Academy of Ophthalmology, Nov. 2013. Accessed Apri. 12, 2023.
10. Turbert D. What is trachoma? American Academy of Ophthalmology. 2022. Accessed April 12, 2023.
11. Trachoma. World Health Organization (WHO). 5 October 2022. Accessed April 12, 2023.
12. World Health Organization. WHO congratulates Benin and Mali for eliminating trachoma as a public health problem. Press release. May 16, 2023.
Related: Priority eye diseases in Africa (Slideshow)
Published: April 17, 2023
Updated: May 16, 2023
© 2023. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content without alteration or modification and subject to attribution as to source.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.