Fibroid: What Every African Woman Should Know
By: Dr. Gbemisola Daramola, MB.BS, MPH, MBA, DFM. Principal Medical Officer, University Health Service, University of Ibadan, Ibadan, Nigeria and DHLA Volunteer Writer, with contribution from the DHLA Team.
.jpg) What is fibroid?
What is fibroid?Fibroid is the most common non-cancerous growths of the uterus (womb) that occur during childbearing years. It is also called uterine fibroid, leiomyoma or myoma. It does not increase the risk of developing a cancer.
Fibroid have been found to be commoner in blacks; Africans and African Americans more than other racial groups.
Experts say that by age 35, about half of black women have had fibroid and by age 50, 80% of them compared to 70% of white women. (1)
The type that you may have depends on the position in relation to the uterus.
The different types are discussed below and illustrated in figure 1:
1. Submucosal Fibroid: The growth bulges into the uterine wall. Grows in the middle layer of the muscle of the uterus. It is the least common fibroid.
2. Intramural Fibroid: The growth is within the muscular wall of the uterus. They are the most common type of fibroid. They can grow large stretching the uterus due to the location.
3. Subserosal Fibroid: the growth projects to the outside of the uterus in the serous membrane. This is the outer lining of all organs and body cavities. They can grow very big and make the abdomen look bigger on one side.
4. Pedunculated Fibroid: It forms when a serosal fibroid develops a stem.
Certain risk factors have been found to predispose to fibroid. These factors (see figure 2) range from genetic predispositions to lifestyle behaviors and include:
1. A positive family history: If you have close family members that have a medical history of fibroid through genetic factors you risk developing fibroid is high.(1)
2. Age: Fibroids do not occur before puberty and are less common after menopause. The earlier the age you start menstruation (menarche) or the later the onset of menopause the greater the risk of you developing fibroid.(1)
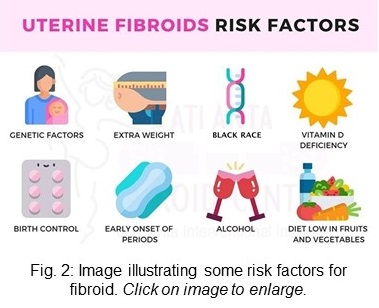 3. Race: Fibroid are commoner in the black race than in any other race
3. Race: Fibroid are commoner in the black race than in any other race
4. Lifestyle factors such as diet vitamin A and D deficiency, high intake red meat, low intake of green vegetables, fruits and fish, increased caffeine and alcohol consumption, smoking, reduced physical activity, and stress in you have a potential effect to increase the format(2,3)
5. Obesity: weight gain increases risk of fibroid only in women who had one or more children.(1)
6. Hypertension and Diabetes: Increase in blood pressure has been found to increase the risk of developing fibroid.
7. Contraceptives and Hormone Replacement Therapy: Estrogen is a hormone that takes care of the womb particularly the replacement of its lining shed every month during menstruation. Progesterone another female hormone prepares the body for pregnancy every month by sustaining the womb to aid the implantation of a fertilized egg. High levels of oestrogen in birth control pills may cause fibroids to develop and grow bigger. Hormone therapy can reduce fibroid symptoms and shrink the fibroids.(1,9)
You may not know you have fibroid. It may be discovered by a doctor incidentally when doing a pelvic examination (the physical examination of the external and internal female pelvic/ reproductive organs). This is because fibroid often cause no symptoms.
The size of the fibroid can determine if it causes symptoms or not.
Fibroid range in size from seedlings not detectable by the human eye to large masses which can be single or multiple, distorting and enlarging the uterus. This enlargement of the uterus can be so much the woman looks as if heavily pregnant with weight gain.
When symptoms occur, they may include some and not necessarily all of the following:
Preexisting fibroid may grow rapidly during pregnancy due to the increased production of some hormones during pregnancy.
However, pregnant women are less likely to develop fibroid.
A study in 2020 showed 20%-40% of all women could develop fibroid but only 0.1%-3.9% of pregnant women do. (4)
Another study in 2010 also showed that 10%-30% of pregnant women with fibroid can develop complications especially if the fibroid is large and in the last two trimesters. 5) Fibroid usually shrinks after pregnancy in most cases.
Fibroid usually require no treatment during pregnancy. If you experience pain or bleeding or threatened preterm labour, bed rest will be prescribed
If you have fibroid, you can still get pregnant naturally. Sometimes the size and type of fibroid particularly the sub-mucosal type that grows into the womb can increase the risk of infertility and miscarriage. Fibroid has been found in 5-10% of infertile patients and the only cause of infertility in 1-2.4 %.(6)
Fibroid can reduce fertility in the following ways:
If you are unable to get pregnant or keep a pregnancy, please see a doctor before concluding that it is caused by fibroid.
If you suspect you have fibroid then you should get a medical examination. Take the following steps:
 See a doctor who may be a primary care doctor or general practitioner or family doctor who will ask about your symptoms and do a pelvic examination, If abnormal changes in the shape or size of the womb is observed, the doctor will send you for further tests.
See a doctor who may be a primary care doctor or general practitioner or family doctor who will ask about your symptoms and do a pelvic examination, If abnormal changes in the shape or size of the womb is observed, the doctor will send you for further tests.
The treatment of fibroid is on individual basis; your symptoms, the size and location of the fibroid, your age, your desire to have a child or not are all put in consideration.
There are 3 main surgical options
1. Hysteroscopic Surgery: For small sized fibroid protruding into the womb, it can be removed by inserting a tube through the vagina into the womb. The fibroid is seen using a camera. It is broken down and removed, No incision is made on the abdomen so in most cases you can go home the same day.
2. Hysterectomy: For women who do not desire to become pregnant, and their fibroid is large in size and causing severe symptoms, hysterectomy is recommended. It is the removal of the womb and it is a permanent treatment for fibroid. It can be done using laparoscopy, through the vagina or making an abdominal incision.
3. Myomectomy: This is an alternative surgery for women who still desire to get pregnant but are having heavy bleeding. It is associated with a risk of recurrence which depends on your age, number of fibroid before the surgery, size of the womb, other coexisting disease and childbirth.
About 15-33% of fibroids recur after a myomectomy and about 10-21% of women who previously had myomectomy have to undergo a hysterectomy within five to ten years later. (8)
The risk of recurrence is higher in women with a family history of fibroid, those with many symptoms and with multiple fibroids. A repeat myomectomy can be done but with each surgery is the increased risk of pelvic adhesion (binding of adjacent organs in the pelvis together) which can lead to more complaints.
Fibroids cannot be prevented. However, research shows lifestyle changes such as reducing high sugar diet, eating fresh fruits and vegetables rich in vitamins C, E and K and regular exercise can reduce the risk. Also reduction of alcohol and caffeine intake and no smoking.
1. Morhason-Bello IO, Adebamowo CA. Epidemiology of uterine fibroid in black African women: a systematic scoping review. BMJ Open. 2022 Aug 3;12(8):e052053. doi: 10.1136/bmjopen-2021-052053. Available from here.
2. Ciebiera M, W?odarczyk M, S?abuszewska-Jó?wiak A, Nowicka G, Jakiel G. Influence of vitamin D and transforming growth factor β3 serum concentrations, obesity, and family history on the risk for uterine fibroid. Fertil Steril. 2016;106(07):1787–1792. Available from here.
3. Paffoni A, Somigliana E, Vigano' P et al. Vitamin D status in women with uterine leiomyomas. J Clin Endocrinol Metab. 2013;98(08):E1374–E1378. Available from here.
4. Eyong E, Okon OA. Large uterine fibroids in pregnancy with successful caesarean myomectomy. Case Rep Obstet Gynecol. 2020 Nov 10;2020:8880296. doi: 10.1155/2020/8880296.Available from here.
5. Lee HJ, Norwitz ER, Shaw J. Contemporary management of fibroid in pregnancy. Rev Obstet Gynecol. 2010 Winter;3(1):20-7. Available from here.
6. Guo XC, Segars JH. The impact and management of fibroids for fertility: an evidence-based approach. Obstet Gynecol Clin North Am. 2012 Dec;39(4):521-33. doi: 10.1016/j.ogc.2012.09.005. Available from here.
7. The Society of Obstetricians and Gyneacologists of Canada. Uterine Fibroid, How are fibroids treated? [Internet, n.d.] Accessed April 19, 2023. Availablr from here.
8. Kramer KJ, Ottum S, Gonullu D, Bell C, Ozbeki H, Berman JM, Recanati MA. Reoperation rates for recurrence of fibroids after abdominal myomectomy in women with large uterus. PLoS One. 2021 Dec 9;16(12):e0261085. doi: 10.1371/journal.pone.0261085. Available from here.
9. Kwas K, Nowakowska A, Fornalczyk A, Krzycka M, Nowak A, Wilczy?ski J, Szubert M. Impact of Contraception on Uterine Fibroids. Medicina (Kaunas). 2021 Jul 16;57(7):717. doi: 10.3390/medicina57070717. Available from here.
Related:
Published: May 8, 2023
Last reviewed: June 20, 2025
© 2023. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.