Self-Care for Diabetic Foot Ulcer in Africa – A Nurse’s Perspective
By Chinonso Cynthia Ukah. BNSc, RN, RM, RPHN. Freelance Health Writer. Medically reviewed by A. Odutola, MB.BS. PhD, FRCSEd.
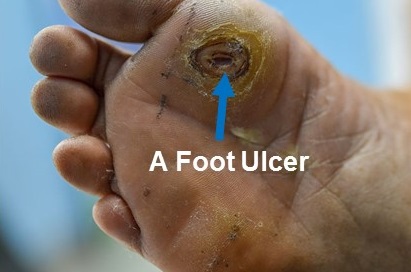
A diabetic foot with a grade 1 foot ulcer. Source.
When Dr. Aliyu said he’d prefer to live with HIV than with diabetes, everyone in his social media group called him dumb until he explained why.
“At least with HIV, you get free medications, non-governmental organisations (NGOs) check up on you, and there’s a public health system in place for care,” Dr. Aliyu said. “With diabetes, you’re on your own until your foot starts rotting.”
Yes, in most African countries where universal health insurance and or public health programs to support diabetics are lacking, people with diabetes have to take personal responsibility for the totality of their healthcare needs. This often translates to individual consequences for African diabetics.
For example, at one Nigerian hospital, five people walked in with small wounds on their feet thinking it was nothing serious. They were shocked to find out they had been living with diabetes for over six years without knowing it. Those small wounds were actually diabetic foot ulcers (DFUs).
Another 28 people only came to the hospital when their wounds were already badly infected and contained pus (Stage 3 - Wagner classification). Some had first tried traditional treatments with hope that the wounds would heal. But they only got worse.
These kinds of stories are common in many low income countries in sub-Saharan Africa (SSA) where about 13 in every 100 people with diabetes develop foot ulcers and many are not aware of the dangers of untreated foot ulcers. DFU is one of the most common reasons for amputations among diabetic patients.
This article will help you understand what diabetic foot ulcers are, how to spot them early, and the right way to care for them.
A diabetic foot ulcer (DFU) is an open wound on any part of the foot of a person with diabetes. It leads to a loss of one or more layers of the skin and in severe cases, may even affect the bones or muscles of the foot. The toes and heels of the foot are mostly affected and the possibility of developing a DFU is as high as 34% over the lifetime of a diabetic patient.
The colour of a diabetic foot ulcer can give you a clue about how well it’s healing or if it’s getting worse. If your wound is:
Foot ulcers are caused by the range of metabolic disorders occurring in diabetes. An interaction of the risk factors below also contribute to diabetic foot ulcer.
1. Previous foot ulcers or amputation: If you’ve had foot ulcers before or have lost a leg because of one, your risk is higher (50%).
2. Diabetic Peripheral Neuropathy (DPN): This is the loss of ability to feel with the feet.
3. Peripheral Arterial Disease (PAD): This means there's reduced blood flow to the feet.
4. Other long-term complications: If you have end-stage kidney disease, are on dialysis, or have had a kidney transplant since being diagnosed with diabetes.
5. Plantar callus: This is a thick, hard skin at the bottom of the foot that forms from dry skin, loss of feeling abilities and repeated pressure on the foot. This can cause ulcers.
6. Elevated foot pressures: If your job requires you to stand or walk for too long, especially without proper footwear.
7. Foot deformity: If your foot has changed shape due to nerve damage or bone problems (e.g. hammer toes, Charcot or flat feet), it makes it more likely to rub against shoes and increase your risk of foot ulcers.
Other risk factors are; feet edema (swelling of the feet), ethnic background and poverty.
There are different staging systems used to classify diabetic wounds. But the one commonly used is called the Meggitt-Wagner Grading System. It has 6 grades as shown in Table 1 and Figure 1 below.
Table 1: Showing the Meggitt-Wagner Grading System for diabetic foot ulcer. Click on imagr to enlarge..
Fig. 1: Pictorial images of Stages of Diabetic Foot Ulcers. A - Stage 1, B - Stage 3 and C- Stage 5. Click on image to enlarge.
The most effective ways to stop a foot ulcer from developing are by keeping your diabetes under good control at all times and practicing daily foot care.
The first thing to do when you notice a blister, cut, or open sore on your foot is to see your doctor. They will prescribe the right wound care materials and may begin treatment with the help of nurses at the hospital.
Following on your doctor’s visit, home care becomes your responsibility and here’s how to do it safely:
1. Wash your hands thoroughly and wear clean gloves.
2. Remove any existing dressing. You are to apply a new dressing every day or when the wound is soaked.
3. Observe the wound. What is its colour? Is it clean, smelly, draining pus or blood? Write any abnormality you observe in a notebook so you can report it to your doctor later.
4. Dip a sterile gauze or cotton wool into normal saline or whatever solution is used to dress the wound in the hospital. Never use spirit, iodine, or soap unless your doctor says so.
5. Clean the center of the wound first. Use as many clean gauzes as possible. If there's a slough (a yellowish, soft layer) and it's removable, clean it off so healing can properly take place.
6. Clean other parts of the feet and toes, especially the spaces between the toes. Make sure it is dry.
7. Apply the prescribed ointment your doctor gave you. Do not apply herbal mixtures, methylated ointment, or any over the counter creams on the ulcer.
8. Cover the ulcer with a dry sterile gauze. Use as many as can absorb the fluid if the wound is draining. Then gently tie with a bandage or medical grade adhesive tape to hold it in place.
9. Always take weight off the injured foot (off-loading). You can use clutches or a wheelchair. Walking directly on the wound worsens it and delays healing.
10. Make sure to eat well and take your insulin or oral medications as prescribed. This is the basis for a proper wound healing.
See your doctor immediately if:
Family and caregivers can support a diabetic with foot ulcers in the following ways:
Conclusion
Diabetic foot ulcers are not small wounds. They can lead to serious infections, amputations, and even death if ignored. Early detection, proper daily care, and support from loved ones or professional caregivers can help many people heal and avoid complications. In many sub-Saharan African countries where access to medical care is limited, learning how to properly manage foot ulcers at home becomes even more important. Don’t wait until the wound gets worse. Take care of your feet every day, follow your doctor’s advice, and ask for help when you need it.
1. Abubakar AI, Sabo VY, Okpako IO, Lawal Y, Mshelia-Reng R, Anumah FO. Surgical management of diabetic foot ulcer in a low resource setting: a Nigerian tertiary hospital experience. Afr J Endocrinol Metab. 2023;13(1):8–12. doi:10.4103/ajem.ajem_10_24. Available from here.
2. Haile KE, Asgedom YS, Azeze GA, Amsalu AA, Gebrekidan AY, Kassie GA. Diabetic foot: A systematic review and meta-analysis on its prevalence and associated factors among patients with diabetes mellitus in sub-Saharan Africa. Diabetes Res Clin Pract. 2025 Feb;220:111975. doi:10.1016/j.diabres.2024.111975. Available from here.
3. Boulton AJM, Whitehouse RW. The Diabetic Foot [Internet]. In: Feingold KR, Ahmed SF, Anawalt B, et al., editors. Endotext. South Dartmouth (MA): MDText.com, Inc.; 2000– [updated 2023 Jul 28; cited 2025 Jun 22]. Available from here.
4. Huang ET, Mansouri J, Murad MH, Joseph WS, Strauss MB, Tettelbach W, Worth ER. A clinical practice guideline for the use of hyperbaric oxygen therapy in the treatment of diabetic foot ulcers. Undersea Hyperb Med. 2015;42(3):205–247. Available from here.
5. Manalu NV, Yunitasari E, Malinti E, et al. How diabetic foot ulcer patients can self-treat wound care: an integrative literature review. SAGE Open Nurs. 2024 Aug 21. doi:10.1177/23779608241274219. Available from here.
Learn more about Diabetes in Africa from here:
Type 1 Diabetes Mellitus: An Explainer for Africans
Type 2 Diabetes: What Africans need to know
You May Have Prediabetes and Not Know. How to Find Out (Tips)
Economic Impact of Diabetes in Sub-Saharan Africa
Published: August 18, 2025
© 2025 Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content freely for non-commercial purposes without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.