Poliomyelitis in Africa: Progress, Challenges, and Road to Eradication
Isma Butt, DPT, DLHA Volunteer and Freelance Medical Writer. Medically reviewed by: Dr. K. Craig. Mb.BS, MPH

Image showing a group of seated African children with polio holding on to their crutches. Credits WHO
Poliomyelitis, commonly known as polio, is an infectious viral disease that has affected numerous families in Africa over the years. This infectious virus has the potential to cause paralysis, disability, and even death, particularly in children less than five years old. However, with incredible work in the field of public health and tremendous vaccination campaigns, Africa is on the verge of eliminating this disease today.
It is important to understand the current situation of polio, the obstacles encountered, and what should be done to eliminate it among people in Africa. This article will take you through the effects of polio, the recent eradication achievements in Africa, the challenges that remain, and the efforts that all stakeholders can make to end the fight. Knowing this will also help you protect yourself, your family and your community.
Poliomyelitis is a contagious illness caused by a special type of germ called poliovirus (enterovirus) which multiplies in the intestine, from where it can get into the nervous system and cause paralysis, or even death
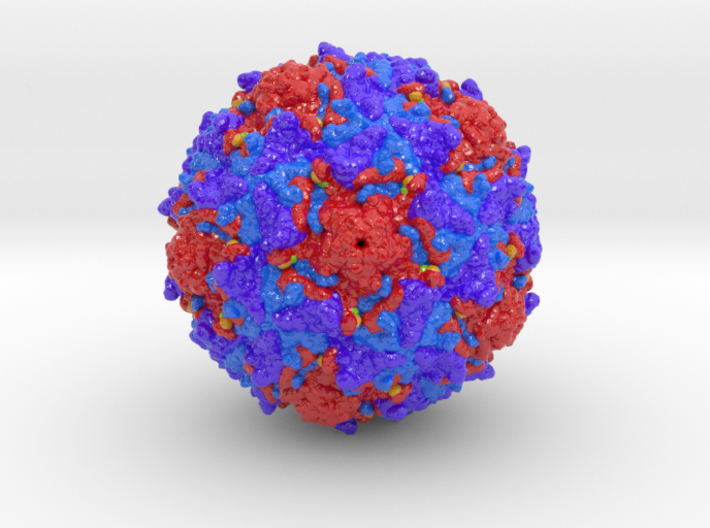
An image showing the poliovirus. Credit
There are three distinct serotypes (variants) of wild polio virus (WPV), types 1, 2 and 3, and infection or immunisation with one serotype does not induce immunity against the other two serotypes.
Of the three wild poliovirus serotypes only WPV1 remains. WPV2 was declared eradicated in September 2015, with the last case detected in India in 1999. WPV3 was last detected in November 2012 in Nigeria and was declared eradicated in October 2019.
Image showing three different variants of poliovirus. Click on image to enlarge
1. Faecal-oral route: This is the primary route of polio transmission. The virus spreads from the faeces (poop) of an infected person to the mouth of another person, which can happen when hands are not properly washed after using the toilet, or through food or water contaminated by the faeces. (see fig. 1):
Fig. 1: Image demonstrating the faecal-oral route of virus transmission. Click on image to enlarge.
2. Oral-oral Route: This mode of transmission is rare and happens when an infected individual coughs, talks, or sneezes, and releases tiny saliva droplets. These droplets then land on the mouth or nose of a nearby person or on objects people touch (utensils, food, etc.) and then place their hands into their mouth. This happens when individuals are in close contact because droplets do not travel very far. Therefore, the transmission can be either through direct contact with saliva or through air droplets near an infected person (see. fig 2). Once inside the body, the virus multiplies in the intestine and can enter the nervous system.
Fig. 2: Image showing the direct droplet (Oral-oral) route of virus transmission. Click on image to enlarge.
About 70% of polio infections in children do not show symptoms. Infected individuals without apparent illness pass the virus through their nose, throat secretions, and poop over days or weeks and can infect others.
1. Abortive poliomyelitis: This is the mildest form and occurs in 25% of cases. It makes you feel sick but does not cause permanent damage. The symptoms feel more like a mild flu which is usually short-lived. Symptoms include:
2. Non-paralytic poliomyelitis: It occurs in 1% to 5% polio infections in children. This type also causes flu-like symptoms but they are more severe and last longer. It can lead to:
Hospital care can be needed, but paralysis does not occur.
3. Paralytic poliomyelitis: This is the rarest and the most severe form of polio seen in less than 1% population. The virus attacks and destroys the nerve cells that control muscles. It leads to permanent paralysis of some muscle groups, e.g., breathing muscles, leg muscles, and death if left untreated.
Photo of a child paralysed by Polio. Credit WHO. Click on image to enlarge.
The highest risk is borne by unvaccinated children younger than five years, because their immune system is not fully developed and they have a higher probability of contact with contaminated environments. This is why it is important to vaccinate children.
Related: Poliomyelitis: What Africans Need to Know
Polio outbreaks were common in African countries for many years. These epidemics left thousands of children paralysed or dead. In addition to the physical burden, polio also caused fear and stigma to the families.
But, this began to change in the late 20th century with the introduction of polio vaccines. Mass immunisation, awareness, and the support of foreign partners also helped to decrease the spread of the virus. Since 1988 the number of polio cases in the world has decreased by more than 99 per cent, with major progress being achieved in Africa.
These efforts have helped in the prevention of the spread of the virus and the protection of millions of children. The accomplishment shows the strength of teamwork and how it can lead to a healthier future for all.
Despite the progress, the battle against polio in Africa is not yet over. The continent continues to struggle with issues that ensure the virus remains active in some areas.
WHO Africa regional reports highlight that as of 2025:
These figures are testament to significant progress as well as the effort yet to be done.
Related:
Ghana Launches Nationwide Polio Vaccination Campaign
Kenya Launches Polio Vaccination Campaign
Africa has many major challenges to overcome before it can achieve a polio-free future. Here are some of them:
All these factors may lead to the problem of delaying the eradication of polio, but once known, they can be used to design superior solutions.
The Africa Regional Polio Eradication Action Plan (2024-2025) sets clear goals:
To meet these goals, the plan focuses on:
This comprehensive approach is crucial for sustainable success.
II. Vaccination Programmes
There's no doubt vaccination remains the most effective weapon against polio. Two types of vaccines are in common use in African countries (see fig. 3):
1. Oral Polio Vaccine (OPV): It is given by mouth, easy to use in mass campaigns, and effective at stopping transmission.
2. Inactivated Polio Vaccine (IPV): This injectable vaccine provides excellent individual protection, particularly important in routine immunisation.
Fig. 3: Side-by-side image of Oral and Inactivated Polio Vaccines. Click on image to enlarge. Credit. GPEI
The typical vaccination schedule includes (see Table 1):
In countries like South Africa, this schedule is common.
Tabe 1: Typical vaccination schedule for polio in some African countries. Click on image to enlarge.
Other countries may use slightly different schedules, for example:

A young African girl is receiving the life-saving oral polio vaccine. Credits. WHO
Related: Childhood vaccines and routine immunization In Nigeria
III. Other strategies driving progress include:
Recent advances are helping in keeping the poliovirus in check better than ever:
These tools make programs more effective and assist in overcoming traditional barriers.
Ending polio is a contribution that each individual can make:
Community support is a key piece of this issue.
Vaccination and surveillance programs are led by African governments, assisted by The Global Polio Eradication Initiative with six partners – the World Health Organization (WHO), Rotary International, the US Centers for Disease Control and Prevention (CDC), the United Nations Children's Fund (UNICEF), Gates Foundation and Gavi, the vaccine Alliance. They raise funds, train health workers, develop and educate health workers, and coordinate cross-border strategies.
Technical and financial support is offered by international partners, which is important to reach out to all the children and respond swiftly to outbreaks.
Eradicating polio is beneficial beyond preventing paralysis:
The lessons learnt during the polio fight also enhance the way African countries tackle other infectious diseases and vaccination campaigns.
Africa has made incredible achievements in the fight against polio. Millions of children are safer today than ever before. Yet, the final steps require persistent effort. Continued vaccination, surveillance, community engagement, proper sanitation, good hygiene practices, and strong leadership will wipe out polio for good.
Together, we can protect our children from this paralysing disease. Let us all commit to vaccinating every child, supporting local campaigns, and spreading awareness. A polio-free Africa is not just a dream; it is within our grasp.
Sources:
1. World Health Organisation (WHO) Africa Regional Office: Highlights of the Polio Response, January–March 2025. [internet. n.d]. Cited August 18, 2025. Available from here.
2. Global Polio Eradication Initiative (GPEI), Africa Regional Polio Eradication Action Plan 2024-2025. [Internet. n.d]. PDF. Cited August 18, 2025. Available from here.
3. Global Polio Eradication Initiative (GPEI). A critical moment for global public health: Polio eradication at the 2025 World Health Assembly. [internet. n.d]. Cited August 18, 2025. Available from here.
4. Boston Children's Hospital. Poliomyelitis Types. [internet.n.d]. Cited August 18, 2025. Available from here.
Published: September 3, 2025
© 2025. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content freely for non-commercial purposes without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.