Ectopic Pregnancy in Tropical Africa: Causes, Symptoms and Treatment
Author: Azuka Ezeike, MBBS, FWACS (Obstetrics and Gynaecology), FMCOG, MSc. (Public Health). Medically reviewed by the DLHA Team

A healthcare professional in blue scrubs performing an ultrasound scan on a woman. Ai Image from ChatGpt
The joy of a positive pregnancy test is beyond measure, especially if the pregnancy was desired. This joy can turn sour if the pregnancy is found to be abnormal. It is even worse if the doctor explains that the condition may lead to loss of a reproductive organ or even life if not treated promptly.
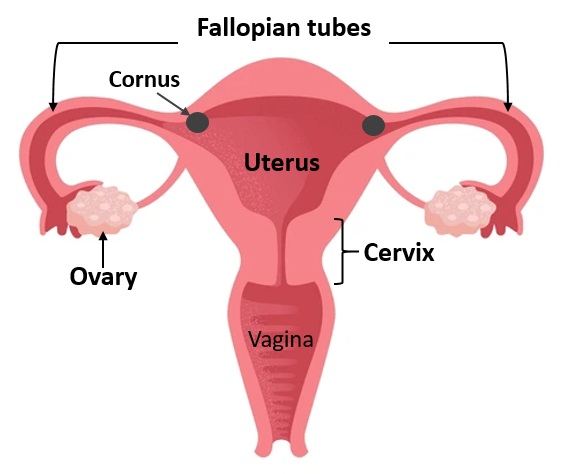
An ectopic pregnancy occurs when the fertilised egg is implanted (attached) outside the uterine cavity (womb), most commonly in the fallopian tube.
Ectopic pregnancy is one of the abnormalities of pregnancy, and the diagnosis is usually associated with distress because of the complications linked to it. In some cases, the complications can be life-threatening, especially when rupture occurs. Early diagnosis and intervention are needed to prevent organ loss or a threat to life.
Rates of ectopic pregnancy in Lagos, Nigeria. Click on image to enlarge. Data source
Ectopic pregnancy happens in about 1-2 out of every 100 pregnancies in the United States. A study in Lagos, Nigeria, found that ectopic pregnancy occurred in about 2 out of every 100 deliveries and caused death in about 1 out of every 100 cases.
In rare situations, an ectopic pregnancy can occur alongside a normal pregnancy. This condition is called a heterotopic pregnancy. It is seen in about 1 in 30,000 pregnancies, but the chances increase with assisted reproductive techniques.
This article discusses the locations, methods of diagnosis, and treatment options for ectopic pregnancy in Africa.
Other sites include:
Ectopic pregnancy can occur without any risk factors; however, some factors can increase the risk (see fig. 2). [3, 4]
Fig. 2: Illustration of some risk factors of ectopic pregnancy. Click on image to enlarge
Your risk may be higher if you:
A study in Accra, Ghana, showed that starting sex early in life, multiple partners, and previous evacuation of the womb also increase risk [3].
Related:
Pelvic Inflammatory Disease in Africa: Causes and Symptoms
Tips on Safe Sex Practice for African Adolescents and Young Adults
The risk factors for ectopic pregnancy in locations outside the fallopian tube are not yet fully understood, but they may be related to some of these factors as well.
For ectopic pregnancies that happen in the fallopian tube, the risk factors increase the chances of the event by: [1]
The fallopian tubes are delicate, tube-like structures on both sides of the womb. This is the place where the sperm meets the egg and fertilisation occurs. They are made up of smooth muscles that contract rhythmically to help move the fertilised egg. They also have cilia, which are tiny, hair-like structures that sweep the egg towards the womb for implantation (attachment).
When the inner lining of the tube (epithelium) or cilia are damaged, often due to infection or previous surgery, the fertilised egg may fail to move properly. A blockage in the tube can also stop the egg’s journey. In such cases, the embryo may implant within the tube, leading to a tubal ectopic pregnancy. The most common site of attachment in the tube is the ampulla (the widest part of the fallopian tube)
In addition, if the smooth muscle contractions are reduced, the transport of the fertilised egg slows down, which can also result in attachment of the embryo to the tube.
As the pregnancy grows inside the fallopian tube, the tube may eventually burst (rupture), leading to bleeding. This usually happens between 6 and 16 weeks of pregnancy, depending on the part of the tube where the pregnancy is attached.
For ectopic pregnancies that occur outside the fallopian tube, the exact mechanisms are less clear. For instance, in rare cases of abdominal pregnancy, it is believed that the fertilised egg may be expelled from the open end of the tube (a process known as tubal abortion) and then attach to organs in the abdominal cavity.
The common symptoms of ectopic pregnancy are shown in Table 1.
Table 1: listing the symptoms of non-ruptured and ruptured ectopic pregnancies. Click on the image to enlarge.
If the ectopic pregnancy is unruptured, it may not cause symptoms, and you may only notice signs of early pregnancy. However, scanty vaginal bleeding may occur at this stage.
Major bleeding often occurs inside the abdomen when an ectopic pregnancy in the fallopian tube ruptures, and you may then experience any of these: [1, 2]
Related: Pregnancy: Symptoms, Test, Types, Stages, Complications, Care and More
Diagnosis involves: [3]
If you have an ectopic pregnancy, you may have missed your period and have one or more symptoms.
To arrive at the diagnosis, your doctor will ask about your symptoms and risk factors.
Your doctor will check:
If you have a ruptured ectopic pregnancy, you may present in shock. Your doctor will quickly diagnose it with an ultrasound scan and rush you to surgery.
Ectopic pregnancies in other sites are more difficult to diagnose. This is because the signs and symptoms are not always clear [5]. If the ultrasound scan does not give a definite answer, doctors may carry out:
These two procedures are used to diagnose and treat the condition.
Sometimes, other conditions can look very similar to an ectopic pregnancy and may confuse the diagnosis. [1].
Fig, 3: Some conditions that can be confused with ectopic pregnancy. Click on image to enlarge.
These include: (fig. 3)
The treatment of ectopic pregnancy depends on several factors, including: [1, 2, 4]
Options include:
This is considered only in rare cases, especially if the hCG level is less than 200miu/ml and continues to decline. In this case, your condition and hCG levels are closely monitored by your doctor. No medication is given.
This involves the use of drugs to treat the ectopic pregnancy. The most common drug is methotrexate. This is a drug which stops cell growth in the developing pregnancy. It is usually given as an injection into the muscle in one dose, two doses, or multiple doses [4].
Your doctor will consider using methotrexate if:
Monitoring may take days and weeks and includes checking of:
If methotrexate treatment fails, surgery may be needed.
If methotrexate is not suitable, Actinomycin D may be used, though with more side effects [4].
In some cases, methotrexate or potassium chloride may be injected directly into the tube alongside surgery.
Surgical treatment involves the treatment of the disease with surgery (operation)
Options include:
A study in Ghana showed that more than 7 out of 10 women came to the hospital after the ectopic pregnancy had already ruptured. This is why, in many parts of Africa, most ectopic pregnancies are treated with salpingectomy.
For ectopic pregnancies in other sites, treatment depends on the location and may involve medical or specialised surgical methods [5].
If you are in early pregnancy or unsure if you are pregnant and develop severe abdominal pain, fainting, or bleeding, call emergency services and see your doctor immediately.
Ectopic pregnancy is an abnormal outcome of pregnancy. In many cases, it requires surgery. Early diagnosis can prevent rupture and help preserve fertility and prevent massive bleeding. With advances in diagnosis, death rates have reduced. If you miss your cycle, see your doctor for an early scan to help detect and diagnose ectopic pregnancy promptly.
Yes. Many women go on to have successful pregnancies. Fertility depends on the health of the remaining reproductive organs. Because the risk of recurrence is higher, early ultrasound in the next pregnancy is advised.
Not always. However, preventing and treating sexually transmitted infections and stopping smoking can help reduce the risk.
1. Vadakekut ES, Gnugnoli DM. Ectopic pregnancy. [Updated 2025 Mar 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 [Cited 2025 Sep 11]. Available from here.
2. Asah-Opoku K, Oppong SA, Ameme DK, Nuamah MA, Mumuni K, Yeboah AO, et al. Risk factors for ectopic pregnancy among pregnant women attending a tertiary healthcare facility in Accra, Ghana. Int J Gynaecol Obstet. 2019 Oct;147(1):120–5. Available from here.
3. Hendriks E, Rosenberg R, Prine L. Ectopic pregnancy: diagnosis and management. Am Fam Physician. 2020;101(10):599-606. Available from here.
4. Mullany K, Minneci M, Monjazeb R, C Coiado O. Overview of ectopic pregnancy diagnosis, management, and innovation. Women's Health (Lond). 2023 Jan-Dec;19:17455057231160349. doi: 10.1177/17455057231160349. Available from here.
5. Sokalska A, Rambhatla A, Dudley C, Bhagavath B. Nontubal ectopic pregnancies: overview of diagnosis and treatment. Fertil Steril. 2023 Sep;120(3 Pt 2):553–62. Available from here.
More related resources:
Common Causes of Miscarriage in Nigerian Women
How To Determine Your Fertile Window For Pregnancy
What Africans Need To Know About The Pregnancy Test and Kit
How to Improve Reproductive Health Wellbeing: Advice for African Adults
Published: October 12, 2025
© 2025. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content for non-commercial purposes without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.