Attention Deficit/Hyperactivity Disorder in African Children
Author: Oluwabukola Janet Adeyeri, MSc. Child & Adolescent Mental Health. Medically reviewed by: A. Odutola, MB.BS, PhD.
Wood block image abbreviation of ADHD on a pink background with an image of four bare chested African children posing together outdoors. Composite picture from Unsplash & Freepik
Attention Deficit/Hyperactivity disorder (ADHD) is a common long term neurodevelopmental disorder that affects millions of children worldwide, yet it’s often misunderstood in African settings. When a child is seen in class or at home constantly on the move, easily distracted, not wanting to complete assignments, or always jumping and refusing to follow instructions in many African countries, the child is often said to be deliberately stubborn, impatient, or even tagged as having a spiritual problem. [1]
These misunderstandings about ADHD lead to late diagnosis, stigmatization, and harsh treatment of children with the disorder. Despite its prevalence, Attention Deficit/Hyperactivity Disorder still remains underdiagnosed and misunderstood in Africa.
This article will provide you with accurate information on ADHD in African children; its cause, risk factors, signs and symptoms, diagnosis, and treatment options. You will also learn why well organised community and national awareness raising are needed about the condition across many African countries.
ADHD is a neurodevelopmental disorder that affects children's daily functioning and development. It starts in childhood and can span through adulthood. Children with this disorder exhibit some patterns of persistent inattention, hyperactivity, and impulsivity and this can continue till adulthood if early intervention is not sought. [2]
ADHD in children may occur in three types (See fig 1):
Fig. 1: Types of ADHD in children. Click on image to enlarge. AI generated image from ChatGpT
The predominantly inattentive type is the most common type of ADHD in Africa and it involves difficulty staying focused, getting easily distracted, and forgetting tasks easily. Children who present with this don’t have symptoms of hyperactivity/impulsivity.
In this type, most symptoms present as hyperactivity and impulsivity, rather than inattentiveness. The child is always restless, talks too much, fidgets, and acts without thinking about the consequences of their actions.
A child with combined ADHD type must exhibit the symptoms of both inattentiveness and hyperactivity/impulsivity.
Fig. 2: Pooled estimate of children and adolescents living with ADHD in Africa. Source
ADHD affects about 3-5% of school aged children globally. A systematic review and meta-analysis estimated that ADHD has a prevalence of 7.47% in children and adolescents living in Africa (see fig. 2) and it is more common in males than in females, with a ratio of 2:1 [2]
The cause or causes of ADHD is/are unknown. The main problem with ADHD children is believed to be due to the dysfunction in the prefrontal cortex. The prefrontal cortex plays a huge role in the brain’s executive functioning like regulating attention, impulse control, planning, and responding to stimulus and children with ADHD find it difficult to perform tasks that demand their optimum attention. [3]
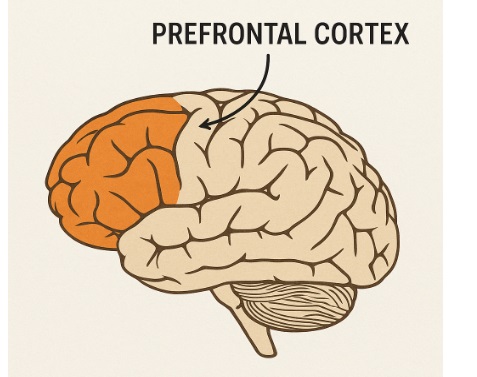
Fig. 3: Cartoon illustration of the left view of the brain showing prefrontal cortex location. AI generated image from ChatGpT
Common risk factors associated with Attention Deficit/Hyperactivity Disorder are:
Common biological risk factors of the condition include:
Social factors surrounding the child or parents can also pose a risk to the child having ADHD. Some of them include:
The symptoms of ADHD in children would have been much present before the age of 12 and must have lasted for at least 6 months.
For a child to be diagnosed with the condition the following symptoms must have been present in more than one setting (including home, school, church, mosque, etc.) and interfered with the child’s daily activities. [7]
These symptoms falls into two categories, which include (see fig. 4):
Fig. 4: ADHD symptoms in children. Click on image to enlarge. AI generated image from ChatGpT.
The child must meet at least 6 out of 9 of these symptoms:
The child must meet six out of nine of the following impulsivity/hyperactivity symptoms:
ADHD is diagnosed clinically using criteria detailed in the Diagnostic and Statistical Manual for Mental Disorders, fifth edition (DSM-5).
The following conditions must be met before a diagnosis can be made by a skilled healthcare provider including any of the following: general practitioner/family doctor, pediatric neurologist, child psychologist, child and adolescent mental health professional, or psychiatrist. [8]
The assessment is done by interviewing the parents, asking questions based on the development of the child from conception till the point of visit. Also, school reports and observations of the teachers will also be put into consideration.
ADHD can be managed effectively with the right interventions to help the child to cope well with family and friends. The two unique ways to treat/manage ADHD are:
This is mostly recommended for parents of and children with ADHD. This is because certain drugs may create adverse effects on kids, particularly if they are younger than five. [9] Behavioral interventions are coping strategies parents and teachers can employ in managing ADHD and improving emotional regulation. Common behavioral therapies include:
2. Pharmacotherapy/medications
For older children above five, medications can be combined with behavioral therapy to help control the symptoms. The medications can either be stimulants (e.g., Methylphenidate and Amphetamine) or non-stimulants (e.g., Atomoxetine, Guanfacine, Viloxacine, and Clonidine). These medications must be prescribed by the child psychologist or psychiatrist because they are in the best position to determine the dosage and adjust medications as time goes by.
If ADHD goes untreated, it can affect children’s perception of themselves and cause them to be withdrawn from others.
Major complications associated with the condition are:
Children in Africa are frequently afflicted with ADHD, a neurobehavioural disorder. There is a need to increase awareness, train healthcare professionals, parents, teachers, and provide resources to support children living with the disorder. With early diagnosis, intervention, and reduced stigma, these children can live a productive and fulfilling life.
A person with ADHD finds it difficult to pay attention, remember things, stay organized, and can be quite restless.
Yes, ADHD is a mental disorder that affects a person’s ability to function due to an impairment in the brain’s prefrontal cortex.
Heredity is one of the prevalent risk factors linked to ADHD. So, it runs in the family if there’s a prior history of ADHD in that family.
ADHD can’t be permanently cured. However, with proper management and treatment, a child with ADHD can also function optimally among his/her peers.
No, they are not the same disorders. ADHD affects a child’s focus, attention, and impulse control while ASD affects a child’s social interaction, communication, and behavior patterns. Despite some similarities, such as sensory impairments and emotional instability, they are still two different conditions. It’s also common for a child to have both disorders (Autism and ADHD). This is because children who present with Autism always have some symptoms of hyperactivity too.
Talk to your primary healthcare provider first if you suspect your child may have ADHD. There are several secondary and tertiary health institutions that offer specialist or advanced assessment, diagnosis, and treatment services for children with ADHD in different African countries. Your primary care provider will assist you to identify a specialist facility near you that will serve the needs of your child. You can also find special schools/facilities that prioritise taking care of children with the condition.
1. Olatunji, Gbolahan et al. “Navigating unique challenges and advancing equitable care for children with ADHD in Africa: a review.” Ann Med Surg (Lond). 2023 Aug 14;85(10):4939-4946. doi: 10.1097/MS9.0000000000001179. Available from here.
2. Ayano G, Yohannes K, Abraha M. Epidemiology of attention-deficit/hyperactivity disorder (ADHD) in children and adolescents in Africa: a systematic review and meta-analysis. Ann Gen Psychiatry. 2020 Mar 13;19:21. doi: 10.1186/s12991-020-00271-w. Available from here.
3. Arnsten AF. The Emerging Neurobiology of Attention Deficit Hyperactivity Disorder: The Key Role of the Prefrontal Association Cortex. J Pediatr. 2009 May 1;154(5):I-S43. doi: 10.1016/j.jpeds.2009.01.018. Available from here.
4. Rattay K, Robinson LR. Identifying Risk Factors for Attention-Deficit/Hyperactivity Disorder (ADHD): a Public Health Concern and Opportunity. Prev Sci. 2024 May;25(Suppl 2):195-202. doi: 10.1007/s11121-024-01667-w. Available from here.
5. Hatch B, Healey DM, Halperin JM. Associations between birth weight and attention-deficit/hyperactivity disorder symptom severity: indirect effects via primary neuropsychological functions. J Child Psychol Psychiatry. 2014 Apr;55(4):384-92. doi: 10.1111/jcpp.12168. Available from here.
6. Soheilipour F, Shiri S, Ahmadkhaniha HR, Abdollahi E, Hosseini-Baharanchi FS. Risk factors for attention-deficit/hyperactivity disorder: a case-control study in 5 to 12 years old children. Med Pharm Rep. 2020 Apr;93(2):175-180. doi: 10.15386/mpr-1407. Available from here.
7. Magnus W, Anilkumar AC, Shaban K. Attention Deficit Hyperactivity Disorder. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from here.
8. Drechsler R, Brem S, Brandeis D, Grünblatt E, Berger G, Walitza S. ADHD: Current Concepts and Treatments in Children and Adolescents. Neuropediatrics. 2020 Oct;51(5):315-335. doi: 10.1055/s-0040-1701658. Available from here.
9. Eiland LS, Gildon BL. Diagnosis and Treatment of ADHD in the Pediatric Population. J Pediatr Pharmacol Ther. 2024 Apr;29(2):107-118. doi: 10.5863/1551-6776-29.2.107. Available from here.
Published: September 8, 2025
© 2025. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content for non-commercial purpose without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.