Robert Jarvik, First Artificial Heart Creator Dies at 79
By: Foluke Akinwalere. Health & Wellness Writer. Reviewed by the DLHA Editorial Team.
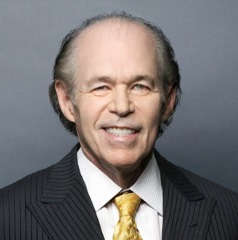
Dr. Robert Jarvik, the First Artificial Heart Creator (May 11, 1946 - May 26, 2025).
Photo Credit: European Academy of Engineering
If you live in Africa and have never heard of Jarvik 7, an artificial heart device, you can be pardoned, but here is your opportunity to learn about the man behind its invention, Dr. Richard Jarvik..
Let’s dive in.
Dr. Richard Jarvik, the brilliant mind behind the first permanent artificial heart used in a human, died at home in Manhattan, New York, USA, from Parkinson’s disease complications on May 26, 2025 at the age of 79; according to statements from his wife, Marilyn vos Savant.
Dr. Jarvik’s legacy lives on in the thousands of patients who have benefitted from artificial heart technology, and in the scientists and physicians he inspired to innovate life-saving medical devices.
Born on May 11, 1946, in Michigan, and raised in Connecticut, his father, a family doctor, influenced his eventual transition into the field of medicine.
But Robert Jarvik didn’t begin his academic journey in medicine. He initially studied architecture at Syracuse University in New York., USA..
A personal family crisis changed the course of his career: his father survived an aortic aneurysm. That event, combined with a strong desire to improve cardiac care, led Jarvik to pivot toward medicine. He later earned degrees in zoology and biomechanics, culminating in a medical degree from the University of Utah in 1976.
Jarvik once said, “I knew that my father was going to die of heart disease, and I was trying to make a heart for him. I was too late.” Rather than becoming a practicing physician, he devoted himself to developing artificial hearts.
Dr. Robert Jarvik is best remembered for designing the Jarvik-7, a permanent artificial heart made from plastic and aluminium. This groundbreaking device was surgically implanted into Barney Clark, a 61-year-old retired dentist, on December 2, 1982. The procedure took place at the University of Utah and was led by Dr. William C. DeVries.
Clark was suffering from severe heart disease and was weeks away from death. Aware of the risks, he volunteered for the operation, hoping that—even if the surgery didn’t save him—it would pave the way for future patients.
During the seven-hour procedure, doctors had to navigate through years of steroid-related tissue damage. After waking up, Clark reportedly told his wife, “Even though I have no heart, I still love you”.
Clark lived for 112 days with the artificial heart, which was powered externally by a 400-pound air compressor. While he never left the hospital and eventually died of an infection, his case demonstrated that humans could, in fact, survive with a machine replacing the heart’s function.
Though Barney Clark’s case was groundbreaking, it was also riddled with challenges. He experienced seizures, kidney failure, and infections. However, the Jarvik-7 was implanted in other patients afterward, some of whom lived longer. Notably:
Despite these milestones, many of the patients suffered complications such as strokes, organ failure, and poor quality of life. This prompted intense public and ethics debate.
By the mid-1980 the Jarvik-7 had become a household name. Media outlets covered it extensively, portraying it alternately as a miracle of modern science and a morally troubling experiment.
Doctors and theologians began to ask serious questions:
In 1990, due to quality control concerns, the U.S. Food and Drug Administration (FDA) halted further approvals of the Jarvik-7. Reflecting years later, Jarvik said in a 1989 interview that pushing for widespread use of the device was “probably the biggest mistake I have made.”
Still, he stood by the broader goal of his work: “These were people who I view as having had their lives prolonged… some were expected to live no more than a week.”
He said,
"I don't think that kind of thing makes a person in medicine want to stop, it just makes you all the more interested in working it through so it can be better.”
Though the original Jarvik-7 was eventually phased out, it laid the foundation for all subsequent artificial heart technologies. The device was eventually succeeded by newer models like the SynCardia Total Artificial Heart, which has since been implanted in more than 1,700 patients worldwide, primarily as a bridge to heart transplantation.
Dr. Jarvik didn’t stop innovating after the Jarvik-7. He went on to develop smaller and more refined heart devices, including:
These devices have helped improve the quality of life for patients awaiting heart transplants or suffering from late-stage heart failure.
In 1985, Robert Jarvik married Marilyn vos Savant, a columnist and author who was once listed in Guinness World Records for having the highest IQ ever recorded. The two became something of a celebrity couple in scientific circles.
Jarvik had two children from a previous marriage and is survived by his grandchildren and siblings.
Though he never practiced clinical medicine, Jarvik’s contribution to the medical field was immense. One of his early artificial heart models even kept a cow alive for 268 days—a precursor to the eventual human trials.
In 2018, Dr. Jarvik received a lifetime achievement award recognising his contributions to cardiovascular medicine. He also appeared in public service campaigns and documentaries promoting the advancement of medical technology.
Dr. O.H. Frazier, a well-known heart surgeon in Houston, praised him by saying, “He had an agile mind and made a great contribution to the care of heart-failure patients.”
Jarvik’s work remains an enduring symbol of what’s possible when innovation, compassion, and perseverance come together to tackle the most complex problems in medicine.
As we honor Dr. Robert Jarvik’s contribution to medicine, we should ask: How can African health stakeholders apply his legacy?
The fight against heart disease in Africa will not be won overnight. But with a mix of public awareness, policy support, local innovation, and global collaboration, heart health can be improved for millions.
From mobile clinics that can help detect early signs of heart failure in far flung communities, to telemedicine platforms that link rural patients to specialists, Africa can be part of the next frontier for cardiovascular care.
Here are some lessons African stakeholders can learn from Jarvik’s legacy:
Jarvik didn’t wait for the perfect system—he saw a problem (heart failure) and created a solution. Africa’s medical innovators, engineers, and researchers must be empowered to dream boldly and act.
Africa needs to train biomedical engineers, fund research, and collaborate with global institutions. With the right infrastructure, Africa can contribute not just to treatment but also to global innovation in heart care
The Jarvik-7 sparked ethical debates. Similarly, Africa’s healthcare innovators must engage with communities, religious leaders, and bioethicists as new inventions are introduced.
Before Africans consider advancing the frontiers of artificial heart devices, they should advocate for and make sure every health facility from primary health centres to tertiary hospitals on the continent never lack basic resources to check blood pressure, run ECGs, and prescribe affordable first line medications for heart health. Innovation must walk hand-in-hand with accessibility to basic care.
Jarvik’s works were widely covered, which helped raise public awareness. African media and public health campaigns must do the same—sharing stories of prevention, treatment, and success in battling heart disease.
Dr. Robert Jarvik’s life work represented a turning point in medical technology and human endurance. The Jarvik-7 artificial heart was more than a machine, it was a symbol of hope for countless people with end-stage heart disease.
Though his invention faced criticism and raised ethical dilemmas, it ultimately opened doors for technological advancements that have saved and prolonged lives. Dr. Jarvik may have passed away, but his vision—to give people more time and better quality of life—will continue to survive him. .
As the world remembers his contributions, one thing is clear: Dr. Robert Jarvik didn’t just build artificial hearts—he transformed heart healthcare globally.
Source:
Edwards I. Dr. Robert Jarvik, Inventor of First Human Artificial Heart, Dies at 79 [Internet]. HealthDay. Last updated 2025 May 30. [Accessed June 1, 2025]. Available from here
You may also like: Dr. Richard Cash: A Global Health Pioneer Transformed Lives with ORT (Oral Rehydration Therapy)
Published: June 5, 2025
© 2025. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use, and share content freely for non-commercial purposes without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.