Lean Type 2 Diabetes Explained To Africans
By Chinonso Cynthia Ukah. BNSc, RN, RM, RPHN. Freelance Health Writer. Medically reviewed by: A. Odutola MB.BS, PhD.

A bare chested young African male wearing blue jeans and checking his waist circumference. Men are higher risk of lean type 2 diabetes because they tend to accumulate more abdominal fat even with a normal body weight. Image credit: Freepik.
It has become common for people to associate diabetes, especially type 2, with obesity. Whether a person has excess fat from birth or gained weight later in life, many people tend to assume that being overweight is the automatic trigger for diabetes.
However, not all fat people develop diabetes, and not all people with diabetes are fat. [1]
In fact, there's a less talked about group - lean individuals with type 2 diabetes. These are people who, despite having a normal or even underweight body size, develop type 2 diabetes mellitus (T2DM). [1] This challenges the stereotype that type 2 diabetes is strictly a “disease of the overweight.”
So, why does this happen? What makes slim individuals at risk for o a condition so strongly tied to excess weight? And what does this mean for diagnosis, treatment, and long-term health?
This article will explain what lean type 2 diabetes means and help you understand how to prevent diabetes in slim individuals.
Fig. 1: Basic definition of Lean Type 2 Diabetes. Click on tmage to enlarge.
Lean Type 2 Diabetes (LT2D) is a form of type 2 diabetes that occurs in adults who are not overweight. These individuals have a body mass index (BMI) less than 25 kg/m², which is considered a normal weight. [2] See fig 1.
Unlike the typical presentation of type 2 diabetes, which is often linked to obesity and high insulin resistance, people with LT2D usually have:
Despite these differences, LT2D still results in elevated blood sugar levels and carries a high risk of complications, especially those associated with the heart.
Globally, the proportion of adults with diabetes who are lean (BMI <25kg/m²) has been rising. A U.S. study revealed that the prevalence of diabetes among lean individuals increased from 4.5 percent in 2015 to 5.3 percent in 2020, while no increase was seen in people who were overweight and obese.
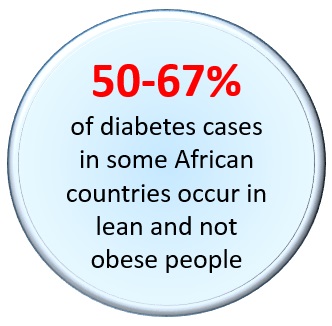
More type 2 diabetes cases in some African countries occur in lean rather than obese people
In sub-Saharan Africa, lean individuals now make up a significant number of diabetes cases. A 2019 study reported that over 50 percent cases of type 2 diabetes occurred in people who are slim and a large portion of these people lived in urban areas. Another study found that in countries like South Africa and Zambia, two-thirds of the diabetic patients studied were lean.
Also, there are observations that diabetes is developing more in slim West Africans than in East and South Africans.
The exact cause of Lean Type 2 Diabetes (LT2D) is not fully understood, but studies point to two major causes:
In LT2D, the pancreas fails to produce enough insulin early unlike the classic T2DM. This failure occurs even before insulin resistance becomes severe. This means that blood sugar rises because insulin is not enough, not necessarily because the body is resisting it. [1]
Researchers have discovered that visceral fat (fat stored deep in the abdomen around internal organs) can exist in people who appear slim. So, while someone may look lean on the outside, they could still have internal fat that triggers mild insulin resistance which contributes to the development of diabetes. [1]
Certain groups of people are more likely to develop LT2D due to genetic, ethnic, and metabolic factors. The key risk groups are shown in Table 1:
Table 1: Key risk groups for Lean Type 2 Diabetes. Click on image to enlarge.
Lean Type 2 Diabetes (LT2D) can be harder to detect because it does not fit the typical presentation of type 1 or 2 diabetes. But the symptoms caused by high blood sugar are still there. The key signs to watch out for are shown in fig. 2:
Fig. 2: Key symptoms and signs of Lean Type 2 Diabetes. Click on image to enlarge.
Diagnosing LT2D can be challenging because it doesn’t present with the typical signs many healthcare professionals associate with type 2 diabetes. After taking your history and performing a physical assessment, your doctor may recommend these tests;
Treatment for LT2D usually involves a combination of medication and lifestyle changes, just like in regular type 2 diabetes. [2] Let's break it down:
Just like classic Type 2 Diabetes, Lean Type 2 Diabetes (LT2D) can lead to serious long-term health complications often with even faster progression because diagnosis has been delayed or missed.
Common complications include:
Table 2: showing summary prevention tips for Lean Type 2 Diabetes. Click on iamge to enlarge.
1. Check your blood sugar regularly especially when you go for checkups. Do not assume that you are safe from diabetes simply because you are slim.
2. Limit the intake of refined carbohydrates and sugary drinks.
3. Eat balanced meals that have low glycaemic index, contain lean protein, whole grains, vegetables, and healthy fats to maintain stable blood sugar.
4. Stay physically active by engaging in regular aerobic and strength-training exercises.
5. Monitor your waist circumference especially if you are a man. A larger waistline may indicate hidden visceral fat, which increases LT2D risk.
6. Sleep well and manage your stress levels. Chronic stress and poor sleep can lead to insulin resistance regardless of your weight.
7. Reduce your intake of alcohol and smoking as both can worsen insulin sensitivity and increase your risk of metabolic disorders.
8. Know your body. If you start experiencing frequent urination, fatigue, blurry vision, or unexplained weight loss, this should prompt a diabetes screening, even if you're slim.
9. If diabetes runs in your family, get screened early and often.
10. Avoid skipping meals
11. Do not engage in extreme or unnecessary dieting in the name of weight loss challenges especially if you are already slim. This can stress the body and impair metabolic function.
12. Participate in local awareness programs like community-based diabetes education
If you are a mother and you are slim,
13. Eat well during pregnancy
14. Prevent and treat malnutrition in your children as early as possible
15. Encourage exclusive breastfeeding for the first 6 months
16. Mothers with a history of gestational diabetes should monitor their children's growth and glucose levels regularly.
Lean Type 2 Diabetes (LT2D) is a lesser-known form of diabetes that affects individuals who are not overweight. Unlike the typical type 2 diabetes that is strongly linked to obesity, LT2D can affect slim and normal weight people and go undetected for years.
One of the biggest myths surrounding diabetes is that being slim means you are safe from diabetes. However, hidden visceral fat, poor early-life nutrition, and genetic factors can trigger this condition even in individuals with a normal BMI. This often leads to missed diagnoses, late treatment, and worse health outcomes. That’s why slim individuals, especially those with a family history of diabetes, signs like fatigue, frequent urination, or unexplained weight loss should not ignore the possibility of a diabetes diagnosis.
Early screening, even in the absence of excess weight, can detect LT2D before complications set in. To prevent LT2D, engage in good nutrition practices early in life, regular physical activity, stress management, and routine health checks.
For mothers, especially during pregnancy, proper nutrition can help reduce long-term diabetes risk in their children.
1. Salvatore T, Galiero R, Caturano A, Rinaldi L, Criscuolo L, Di Martino A, et al. Current knowledge on the pathophysiology of lean/normal-weight type 2 diabetes. Int J Mol Sci. 2022;24(1):658. doi:10.3390/ijms24010658. Available from here.
2. Ogunjobi TT, Adeyanju SA, Akinwande KG, Obasi DE, Aigbagenode AA, Musa A, et al. Improving the prevention and treatment of Lean Type 2 Diabetes in Sub-Saharan Africa: A review. Eur J Sustain Dev Res. 2025;9(2):em0287. doi:10.29333/ejosdr/16288. Available from here.
3. George AM, Jacob AG, Fogelfeld L. Lean diabetes mellitus: An emerging entity in the era of obesity. World J Diabetes. 2015;6(4):613–620. doi:10.4239/wjd.v6.i4.613. Available from here.
Related:
Type 1 Diabetes Mellitus: An Explainer for Africans
Type 2 Diabetes: What Africans Need to Know
Diabetes in Pregnancy in Sub-Saharan Africa: An Overview
You May Have Prediabetes and Not Know. How to Find Out (Tips)
Management of Type 2 Diabetes in Nigeria
Childhood Diabetes in Sub-Saharan Africa: Type 1
Type 2 Diabetes Mellitus in African Children
Published: September 3, 2025
© 2025. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content freely for non-commercial purposes without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.